A new look at implants
The clinical and economic benefits of early loading and cement-retained implant restorations
By Carl J. Drago, DDS, MS, and Anita Daniels, RDH
A two-stage threaded titanium root-form dental implant was first introduced in North America by Branemark in 1983. The original protocol called for unloaded healing of implants that required anywhere from four to six months, as well as two distinct surgical procedures. Original implant restorations consisted of gold cylinders fastened to abutments that were fastened to implants. This protocol involved components and techniques foreign to conventional dentistry such as screws, implant hexes, implant/abutment impression copings, etc. Implant dentistry in the 21st century now combines implant dentistry with conventional techniques, including intraoral preparation of abutments, impressions of the prepared abutments, and cementation of crowns to the prepared abutments.
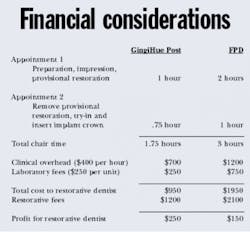
The purpose of this article is to describe a paradigm shift in restoring dental implants, compared to the original implant protocol versus conventional dentistry. It will also illustrate the positive economic impact early loading of dental implants can have on restorative practices.
The potential market for implants in the U.S.
Predictable and long-term replacement of missing teeth with dental implant restorations is but one example of progress within the dental profession. It is well known that edentulous jaws continue to resorb once the natural teeth are lost. Edentulous patients generally experience progressive difficulties in managing complete dentures. Edentulism will continue to be a long-term healthcare issue for decades to come. Douglass et al have performed complex statistical analysis of edentulism and have speculated that the number of people in the United States who will need complete dentures will increase over the next 20 years despite an anticipated decline in the age-specific rates of edentulism. More than 10 percent of adults over 18 years old and 44 percent of people over 75 years old are edentulous. Only 30 percent of adults over 18 have 28 natural teeth and the average 50-year-old male is missing 12.1 teeth. More than 80 percent of the U.S. population is missing at least one tooth, and only 20 percent of have elected to replace any missing teeth. It may be extrapolated that Americans are missing millions of teeth and less than 1 percent of the potential market for tooth replacement has been treated.
Dental implants in general practice
A significant number of general dentists in the United States have incorporated dental implants into practice. According to a recent article in Dental Products Report (2000), "...more than three out of four U.S. general dentists (78 percent) currently restore implants surgically placed by another practitioner." This represents a greater than twofold increase from a similar survey in 1987 (see table 1).
In a recent article in Dental Economics, Ganeles also reported a significant interest in single tooth implant restorations. Approximately 98 percent of recently trained periodontists and 99 percent of recently trained oral and maxillofacial surgeons place dental implants. Fourteen percent of general practitioners place or restore dental implants. The vast majority of all respondents (GPs, periodontists, oral surgeons, and prosthodontists) have suggested implants for patients missing individual teeth. However, GPs are the least successful in getting patients to undergo individual tooth replacement with dental implants.
null
Patient considerations in dental implant treatment
Grogono (1989) surveyed edentulous patients who had been treated with osseointegrated implants and restored with implant supported/retained prostheses. Patients reported the following improvements after being treated with dental implants compared to their original pre-operative (non-implant) condition:
- Better eating—82 percent
- Better speaking—65 percent
- More smiling—49 percent
- Increase self-confidence—54 percent
A significant number of patients would repeat the entire treatment process, if needed (88 percent) and believed that implant treatment was worthwhile (97 percent).
With the proven success of dental implants, why are more implants not being placed and restored by American dentists? One reason for the lack of increasing numbers of implants being placed may be that patients choose not to undergo the procedures associated with implant dentistry. Implants have traditionally been placed using a two-stage surgical technique. This means that patients have had to undergo two surgical procedures, two post-operative periods, the morbidity associated with the surgical procedures and, possibly, two separate doses of antibiotics. Kent (1992) found that one of the major motivating factors for edentulous patients undergoing implant surgery was related to the difficulties associated with eating and denture fit. He found that edentulous patients who could no longer manage wearing complete dentures were the most likely to undergo implant surgery. Akagawa (1988) also reported that dissatisfaction with unstable dentures and discomfort were major motivating factors for patients electing to undergo treatment with dental implants. Phonetics, chewing ability, and esthetics were not found to be motivating factors for patients to choose implant treatment. Akagawa also reported that the fear of surgery was the most important factor for patients deciding against dental implants. Financial considerations, while important, were not nearly as important as the fear of surgery for the patients in these studies.
Another consideration for clinicians and patients electing to forego treatment with dental implants may be the total treatment time associated with the original two-stage surgical protocol:
- diagnosis
- treatment planning
- surgical placement
- soft tissue and bone healing (osseointegration — four months in the mandible, six months in the maxilla)
- surgical uncovering of the implants with abutment connection
- soft-tissue healing associated with uncovering the implants (four to eight weeks)
- restorative procedures (impressions, laboratory procedures — four to eight weeks)
- insertion of the definitive prosthesis
In the traditional two-stage surgical protocol, it would not be unusual for this process to take nine months to a year. These healing periods were originally thought to be necessary to prevent the development of a fibrous capsule around the dental implants. It was also thought that fibrous encapsulation was related to premature loading of the dental implants.
New considerations in implant dentistry: Early loading of dental implants
As the collective dental implant experience of clinicians and researchers around the world has increased, principles that were once thought to be critical for osseointegration have been re-evaluated and modified or eliminated. One such concept involves "early loading" of dental implants. Lazzara et al. conducted a multi-center (10 centers) prospective study involving 429 OSSEOTITE® implants, placed in 155 patients. Implants were loaded 2.1 +/- 0.7 months following placement. A single-stage surgical protocol was followed with either surgical indexing at the time of implant placement or final impressions four to six weeks after placement. Seven of the 429 implants failed to integrate. The cumulative survival rate was 98.5 percent at 12.6 months. These preliminary results suggest that functional loading of OSSEOTITE® dental implants are possible at two months following non-complicated implant placement. It has been the authors' experience that patients more readily accept implant treatment with the above reduced healing times.
Restorative considerations for cement-retained implants restorations
Early reports described failures involving screw fractures, loose screws, and abutment/crown loosening of 30 to 45 percent. It was difficult for dentists to propose implant-retained crowns for patients with success rates of approximately 65 percent. Broken screws and loose implant restorations were quite costly to both the dentist and the patient. It was much more predictable for dentists to propose 3-unit fixed partial dentures (FPDs) to replace a single missing tooth.
Cement-retained implant restorations now enjoy high levels of success in terms of long-term function and aesthetics. Gold electroplated abutment screws (such as Gold-Tite™ Abutment Screws from Implant Innovations, Inc., in Palm Beach Gardens, Fla.) torqued to appropriate levels that precisely fasten machined abutments to implants, provide great predictability to cement-retained implant restorations. Retrievability of retaining screws was once thought to be important because of the propensity of retaining screws to loosen. Improvements in technology have probably made retrievability a non-issue in current clinical practice.
Perhaps the most notable advantage of cement-retained implant restorations is optimal esthetics because cemented crowns cover screw access openings. There has also been discussion relative to a less precise fit between custom abutments and cement-retained crowns. In a study by Guichet et al, they found marginal openings between cemented FPDs and custom abutments were similar before and after cementation. However, the marginal openings between screw-retained FPDs and abutments were significantly smaller after screws were tightened with the screw-retained FPDs. They also found that cement-retained FPDs exhibited a more equitable stress distribution to the implants than did screw-retained restorations.
Restorative considerations: Screw mechanics
Screw loosening has been reported most frequently with single-unit restorations. Implant manufacturers have developed numerous products and technologies to decrease/eliminate screw loosening — anti-rotational design changes for abutments/implants, screw design and material changes, lubrication compounds for screw threads, and torque-controlling devices.
The abutment/implant connection is called a screw joint. The abutment screw will loosen only if the forces trying to separate the screw joint are greater than the ability of the screw to keep the components together; that is, the joint separating forces are greater than the clamping forces of the screw joint. Clinicians who favor using cement-retained crowns for their implant restorations must rely on the integrity of the screw joint between the abutment and the implant for long-term clinical success of their restorations. If the abutment screw becomes loose and the clinician is not able to remove the crown from the abutment to gain access to the screw, the clinician would have to section the crown, remove it, tighten the screw, and make another crown. This would be costly in terms of time and money.
Clinical problems associated with abutment screw loosening have been largely eliminated with the use of dry lubricants, optimal preload, and precise manufacturing of implant components. Cement-retained crowns can be accomplished with predictability, profitably, and in a timely fashion with the use of prepable titanium abutments. The procedures involved combine the technological advances of implant dentistry with the time-tested techniques of conventional fixed prosthodontic treatments.
Preppable titanium abutments
Cement-retained implant restorations can now be fabricated with techniques and materials associated with conventional fixed prosthodontic therapy. This is especially true if the implant surgeon places the appropriate abutment after osseointegration has occurred. (Figure 1, below) In this technique, the surgeon places the abutment after osseointegration has been achieved and torques the abutment screw to the manufacturer's suggested level. The patient would then be discharged to the restorative dentist for fabrication of the definitive crown (Figure 2, below).
null
null
GingiHue™ Posts (Implant Innovations, Inc.) are titanium abutments manufactured with a gold-nitride (TiN) coating. The TiN coating is created with a plasma coating process in which titanium and nitrogen ions are combined. These molecules are bonded to the titanium GingiHue Posts. The gold color provides increased "warmth" to the implant site by eliminating the gray metallic colors associated with titanium abutments (Figure 3, below). The GingiHue Post is attached to the implant with a Gold-Tite Abutment Screw that is tightened to 35Ncm of torque with a restorative torque indicator. When the appropriate torque is applied to the Gold-Tite Abutment Screw, the screw achieves 75 percent greater pre-load than conventional abutment screws. This results in a reduced propensity for screw loosening, screw breakage, and subsequent restorative failure.
null
GingiHue Posts are also fabricated with the Gold Standard ZR™ feature. ZR is an abbreviation for Zero Rotation. Micro-stops are machined into the corners of the abutment internal hexes. These micro-stops are responsible for the precise fit that exists between abutments with the ZR feature and implants by eliminating micro-movement between the abutment and implant. This is important for clinicians because screw loosening can be virtually eliminated.
null
Clinical case/implications
An early-loading single stage surgical protocol can dramatically reduce implant treatment times and increase patient acceptance. The patient missing one tooth can have the implant placed in the surgical office at day one. He or she leaves the office with the soft tissues sutured around the healing abutment that was placed onto the implant. The soft tissues will heal over the next six weeks. The patient generally only has to return once to the surgical office approximately seven to 10 days after implant placement for suture removal and then approximately six weeks after the original surgical appointment for assessment of the health of the soft tissues surrounding the healing abutment, and the stability of the implant. The surgeon removes the healing abutment and places the appropriate GingiHue Post onto the hex of the implant. The selection of the appropriate abutment has already been discussed with the restorative dentist. A radiograph is taken to ensure that the abutment is completely seated onto the implant hex. The abutment screw is torqued to 35 Ncm with a torque indicator and the patient is discharged to the restorative dentist's office.
The patient presents to the restorative dentist's office for abutment preparation, definitive impression, shade selection, and fabrication of the provisional crown. This appointment generally takes about an hour. Typically, patients do not need local anesthesia as they are not having the adjacent teeth prepared. Additionally, the patient did not have to have a 3-unit fixed provisional restoration fabricated and cemented onto the abutment teeth adjacent to the edentulous space. The impression is poured using conventional fixed prosthodontic techniques and materials to fabricate a master cast. Implant impression copings and implant analogs are not required. The master cast is pinned as if the implant abutment was a prepared natural tooth.
The work order is written and the casts are sent to a commercial laboratory for crown fabrication. Generally speaking, commercial laboratories do not have an implant surcharge because all of the laboratory procedures are consistent with conventional fixed prosthodontics. The laboratory returns the crown to the dentist for try-in and cementation.
The patient presents to the restorative dentist's office for removal of the provisional restoration and try-in of the porcelain/gold crown. The dentist will treat this implant and abutment as if it was a natural tooth — adjust interproximal contact areas, evaluate marginal fit, adjust occlusion in centric and eccentric excursions, evaluate for shade matching, and obtain the patient's approval prior to cementation. The crown is polished in conventional fashion and cemented with permanent crown and bridge cement.
Summary
Patients may have individual teeth replaced with implant restorations in approximately 12 weeks — six to eight weeks for osseointegration of the implant, and four weeks for preparation, impression, and fabrication of the definitive crown. In the majority of cases, a patient may require a total of four or five appointments (surgical and restorative) for completion of a long-lasting, esthetic, and functional restoration. What was once considered to be a time-intensive, complex procedure has been modified to a procedure that can be accomplished in a time frame similar to that associated with replacement of a single tooth with a fixed partial denture. Treatment complexity has been significantly reduced with the use of precise, machined titanium abutments that can be prepared intraorally with a high-speed handpiece. The actual cement-retained implant crown is then fabricated with conventional materials and techniques.
All of the restorative procedures described above are familiar to the vast majority of restorative dentists in the United States. A lot of the mystique of implant dentistry has been removed. This should result in an increase in implants being placed and restored in the United States.
Note: References available upon request.
Dr. Carl J. Drago became a Diplomate of the American Board of Prosthodontics in 1984. Dr. Drago is also a Fellow in the American College of Prosthodontists. Dr. Drago has extensive experience on both clinical and instructional implant restorative dentistry. He can be reached at (608) 782-7300, Ext. 2714.
Anita Daniels, RDH, has more than 15 years of clinical experience in periodontics and implant dentistry. She is a member of the Academy of Implant Dentistry, the first dental hygienist to be granted "Active Member" status of the Academy of Osseointegration. For more information, call (800) 443-8166, Ext. 6807.