Oral health is a cornerstone of overall health—a new perspective
When we think of oral health, the immediate association often revolves around dental health and fresh breath. While these are undoubtedly important, a beautiful smile hides deeper dimensions. Studies show that a balanced oral microbiome is crucial for a person’s overall health and even mental well-being.
Over the years, oral health has been somewhat overshadowed in discussions about well-being. While sleep, exercise, nutrition, and stress management, for example, have been seen as important contributors to health, oral health has not received the same attention. However, recent studies and expert opinions are starting to change attitudes. This is reflected in the rise of oral health as one of the six pillars of health in lifestyle medicine.1
Like sleep deprivation, poor oral health puts individuals at risk for conditions such as metabolic syndrome, heart disease, and depression. Studies show that oral infections can contribute to many physical illnesses and even lead to premature death.2
So, how does oral health relate to overall health? Research shows that the balance of the oral microbiome is crucial for oral health and has a significant impact on how the body responds to various diseases.
An imbalance in the oral microbiome, or dysbiosis, can lead to a wide range of health problems—from common dental problems to serious diseases such as cardiovascular disease, diabetes, and even Alzheimer’s disease.3,4 Researchers have found that dental infections can even increase the risk of developing cancer. A recent study found a link between oral bacteria and the development of bowel cancer.5
Inflamed gums: A direct gateway for bacteria to enter the body
Jukka Meurman, professor emeritus of oral and maxillofacial diseases at the University of Helsinki and former head physician at the department of oral and maxillofacial diseases at Helsinki University Hospital, says, “Although oral health is already recognised in professional circles as an important component of both physical and mental health, there is still room for improvement in public awareness.”
He stresses the importance of rapid treatment of oral infections, as bacteria in the mouth can enter the bloodstream and cause infections throughout the body. These infections can lead to a low-grade inflammatory condition that can affect overall wellness. Meurman points out that oral infections are particularly harmful for people with chronic illnesses such as diabetes, rheumatic and kidney diseases, and immune disorders. The increased risk of oral diseases also applies to people taking immunosuppressive drugs, which can predispose them to oral infections such as gingivitis and periodontitis.
“In addition, immunosuppressive drugs can cause mucosal changes such as mouth ulcers and xerostomia (dry mouth), which increases the risk of tooth decay,” Meurman says.
Gum disease is at the root of many health problems
Gingivitis is a common oral infection, which, in its most severe forms, can lead to periodontitis or peri-implantitis—diseases that affect the supporting structures of the teeth and dental implants. Gum infections are caused by oral bacteria, and risk factors include poor oral hygiene, smoking, stress, or systemic diseases.
Periodontitis manifests itself as red, bleeding gums and bad breath, and can progress if not treated carefully. Peri-implantitis describes a condition in which the tissue around an implant with a dental crown becomes inflamed. This inflammation can affect the attachment of the implant and even cause it to become loose if not treated properly. To avoid more serious complications, it is important that gingivitis be detected and treated at an early stage. Regular dental checkups and good oral hygiene habits are an important part of overall health care and can help prevent gingivitis from developing and progressing to periodontitis or peri-implantitis.
Meurman says, “Good oral hygiene and close contact with your dentist always pays off. International calculations show how expensive neglect of oral hygiene is for society and individuals. Dental diseases can spread quickly and require extensive treatment if not treated promptly. Prevention is always the cheapest option.”
Traditional oral hygiene methods are not always enough to keep the mouth healthy, however. Flossing or brushing can be difficult because of age or injury, leaving the spaces between teeth uncleaned. Even if brushing is successful, studies have shown that an effective electric toothbrush only removes about 65% of harmful bacteria in the mouth.6
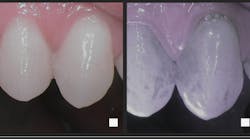
To combat this residual plaque, which is invisible to the naked eye, Finnish researchers have developed an antibacterial method for enhanced oral hygiene based on antibacterial light-activated therapy. Known as Lumoral (not yet available in the US), the method kills both the bacteria that cause tooth decay and the bacteria that cause gingivitis. The Finnish Association of Oral Hygienists recommends its use.7,8
The antibacterial method uses a mouthpiece that activates the antibacterial effect of a mouth rinse (Lumorinse). While similar light-activated antibacterial treatments have been utilized in various dental clinics, the challenge has often been the associated cost and the frequency of required sessions to achieve significant benefits. Home-administered antibacterial treatment enhances dental self-care, particularly in cases where traditional methods prove insufficient or when an existing oral condition demands more comprehensive measures beyond standard brushing and flossing.
Editor’s note: This article first appeared in Clinical Insights newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles and subscribe.
References
- Jaqua E, Biddy E, Moore C, Browne G. The impact of the six pillars of lifestyle medicine on brain health. Cureus. 2023;15(2):e34605. doi:10.7759/cureus.34605
- Kim JK, Baker LA, Davarian S, Crimmins E. Oral health problems and mortality. J Dent Sci. 2013;8(2):10.1016/j.jds.2012.12.011. doi:10.1016/j.jds.2012.12.011
- Maier T. Oral microbiome in health and disease: maintaining a healthy, balanced ecosystem and reversing dysbiosis. Microorganisms. 2023;11(16):1453. doi:10.3390/microorganisms11061453
- de Araújo Silva DN, Casarin M, Monajemzadeh S, de Brito Bezerra B, Lux R, Pirih FQ. The microbiome in periodontitis and diabetes. Front Oral Health. 2022;3:859209. doi:10.3389/froh.2022.859209
- Ray K. A crucial Fusobacterium nucleatum clade in colorectal cancer. Nat Rev Gastroenterol Hepatol. 2024;21(6):375. doi:10.1038/s41575-024-00930-3
- Aggarwal N, Gupta S, Grover R, Sadana G, Bansal K. Plaque removal efficacy of different toothbrushes: a comparative study. Int J Clin Pediatr Dent. 2019;12(5):385-390. doi:10.5005/jp-journals-10005-1669
- Pakarinen S, Saarela RKT, Välimaa H, et al. Home-applied dual-light photodynamic therapy in the treatment of stable chronic periodontitis (HOPE-CP)—three-month interim results. Dent J (Basel). 2022;10(11):206. doi:10.3390/dj10110206
- Liu Y, Qin R, Zaat SAJ, Breukink E, Heger M. Antibacterial photodynamic therapy: overview of a promising approach to fight antibiotic-resistant bacterial infections. J Clin Transl Res. 2015;1(3):140-167.
Tips for gum health for dental professionals
By implementing the following tips, dental professionals can effectively support their patients in achieving and maintaining optimal gum health, reducing the risk of gum disease, and improving their overall oral health.
Educate patients on proper oral hygiene
- Teach patients the correct brushing techniques, emphasizing the use of a soft-bristled toothbrush and the importance of brushing at least twice a day.
- Demonstrate the proper way to floss, ensuring that patients understand how to clean effectively between teeth and along the gumline.
Promote regular dental visits
- Stress the importance of routine checkups and professional cleanings every six months.
- Highlight the role of these visits in the early detection and prevention of gum disease.
Recommend appropriate products
- Suggest effective dental care products such as high-quality electric toothbrushes, fluoride toothpaste, and interdental brushes.
- Stay updated on the latest advancements in dental care, including the latest preventative technologies and antibacterial treatments to help reduce plaque and bacteria in the mouth.
- Educate patients on the benefits of the latest dental technologies and incorporate them into your practice to enhance patient care.
Emphasize the importance of a healthy diet
- Advise patients about the impact of diet on oral health, recommending foods rich in vitamins and minerals, particularly vitamin C and calcium.
- Encourage patients to limit sugar intake to reduce the risk of plaque formation and gum disease.
Offer smoking cessation support
- Provide resources and support for patients looking to quit smoking.
- To motivate patients, explain the harmful effects of smoking on the gums and overall oral health.
Offer personalized patient care
- Develop individualized care plans based on each patient’s specific needs, risk factors, and oral health status.
- Monitor patients’ progress and adjust care plans as necessary, providing personalized advice and treatment options.
Provide posttreatment care instructions
- Ensure patients receive clear instructions on how to care for their gums after dental treatments/procedures.
- Follow up with patients to check on their progress and address any concerns or questions.
Encourage hydration and saliva production
- Advise patients to drink plenty of water to maintain oral hydration and promote saliva production, which naturally protects gums.
- Suggest sugar-free gum or lozenges to stimulate saliva flow in patients with dry mouth.
Promote consistent oral health routines
- Encourage patients to establish and maintain consistent daily oral health routines.
- Provide tools such as reminders or educational materials to help patients stay on track with their oral hygiene practices.
About the Author

Nina Garlo-Melkas, MSc
Nina Garlo-Melkas, MSc, is a health and science journalist.