What I thought would be a routine first dental visit on a 12-year-old male turned into something that had his mom looking at me with pleading eyes to help her son, who clearly was not in a good way.
These are the moments when we must be on our game. We have to examine, diagnose, treat, and subsequently comfort and reassure our patients of their situation. We need to immediately recall what we’ve been taught and successively apply it to clinical situations.
Case presentation
This 12-year-old presented with his mom for a dental visit. The chief complaint was that he was not feeling well, his mouth hurt, he couldn’t eat, it was painful to swallow, and he’d missed out on the last week of school. In general, his health history was unremarkable, temp was low-grade (99.8), and despite not being 100%, he was a trouper. Fist bumps, kiddo.
My hygienist had taken radiographs prior to me coming in.
Pathology point no. 1
Diagnosis: Mesiodens tooth
For a recap on mesiodens teeth, diagnosis, and treatment, please refer to another case report I wrote that you might find of interest. Here is a quick- The lesions may occur “as single, multiple, unilateral, or bilateral (lesions); the presence of multiple supernumerary teeth is called ‘mesiodentes.’”1
- By way of appearance, they typically manifest in a conical- or peg-shaped form.2
- In general, supernumerary teeth—also referred to as hyperdontia or extra teeth—can occur in any location, but they are more prevalent in the maxilla (90%) as opposed to the mandible (10%).2
- The most common type of supernumerary teeth are mesiodentes.1 Their etiology remains unclear, although it is theorized that they are either an isolated finding or part of a “syndrome, specifically cleft lip and palate, cleidocranial dysostosis, and Gardner’s syndrome.”1
- Diagnosis is primarily via radiograph and can be confirmed by taking multiple angles using intraoral and extraoral radiographs (i.e., panoramic, periapicals, etc.). Furthermore, three-dimensional CBCT scans allow dialing in on the palatal location of the mesiodentes and their relationship to adjacent teeth. Delayed or altered eruptions of adult dentition also give rise to the suspicion of mesiodentes. Other common signs include cyst formation and crowding.
- Treatment of mesiodens varies. Although typically asymptomatic, they are “often extracted for aesthetic reasons, to allow the eruption of other teeth, orthodontic reasons, and/or suspected pathology.”3
Pathology point no. 2
Note: The pictures are not of the highest quality as the patient was in extreme discomfort when I took them.
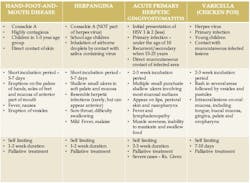
Differential considerations include:
Definitive diagnosis is likely one of two: Herpangina or acute primary herpetic gingivostomatitis
The saying “nothing is for certain unless it’s in a petri dish” stands true in all pathology cases, including this one. However, based on the symptoms and clinical presentation, I was able to surmise that it was more than likely either herpangina or APHG, although I’m leaning toward APHG.
Prescriptions include:
For my patient, I prescribed Magic mouthwash, told him to rest (mom was on board with that), keep his oral cavity as clean as possible (several of my patients have found a diluted Listerine or chlorhexidine rinse to be helpful, but not all can tolerate it), and let it run its course. Mom was to contact me if it didn’t start to improve or get better after 10–14 days.
Pathology refresher
Here is a quick go-to reference tableHere are some additional informational tidbits on the Coxsackievirus and herpesvirus4
Coxsackievirus (for herpangina)
- Picornavirus family (largest and most prevalent of RNA viruses)
- Includes rhinoviruses of the common cold
- Portal of entry via oropharynx and gastrointestinal tract
- Two types: A and B
o Type A includes herpangina, hand, foot and mouth disease, and lymphonodular pharyngitis.
o Type B causes GI illnesses, pericarditis, and myocarditis.
Herpesvirus (includes herpes simplex 1 and 2, acute primary herpetic gingivostomatitis, varicella zoster virus, Epstein-Barr virus, cytomegalovirus, human herpesvirus)
- HSV-1 (primary lesions above the waist), HSV-2 (primarily lesions below the waist, 10% crossover)
- Enters the body through breaks in the skin
- Primary infection followed by latency
- Neurotropic—infects the peripheral nerves and migrates to regional ganglion and remains dormant, therefore protected
- Activated by emotional stress, trauma, cold, sunlight, gastric upset, fever, menstrual cycle, and other factors that result in immune system depression
Keeping it real, raw, and everyday...
Dr. Stacey
References
- Meighani G, Pakdaman A. Diagnosis and management of supernumerary (mesiodens): a review of the literature. J Dent (Tehran). 2010;7(1):41-49.
- Sapp JP, Eversold LR, Wysocki GP. Contemporary Oral and Maxillofacial Pathology. Mosby; 1997:4-5.
- Hyperdontia. Wikipedia. Updated May 5, 2020. Accessed March 15, 2020. https://en.wikipedia.org/wiki/Hyperdontia
- Wood NK, Goaz PW. Differential Diagnosis of Oral and Maxillofacial Lesions. 5th ed. Mosby; 1997:73-74, 167-168.
Editor’s note: This article first appeared in Through the Loupes newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles and subscribe to Through the Loupes.
About the Author
Stacey L. Gividen, DDS
Stacey L. Gividen, DDS, a graduate of Marquette University School of Dentistry, is in private practice in Montana. She is a guest lecturer at the University of Montana in the Anatomy and Physiology Department. Dr. Gividen has contributed to DentistryIQ, Perio-Implant Advisory, and Dental Economics. You may contact her at [email protected].