Management of a complex lower second molar: discussion of a clinical case
By Richard E. Mounce, DDSThe patient pictured in Fig. 1 was referred by his general practitioner for completion of a previously accessed endodontic treatment on No. 18. The tooth had been started approximately two weeks prior. A subsequent second visit ended without the treatment being finished. Prior to the initial access, severe caries at the mesial of the tooth necessitated the root canal. The patient reported difficulty getting numb at both appointments. It is unknown specifically why the case was referred (other than to complete it), and/or why it was not completed in one visit.
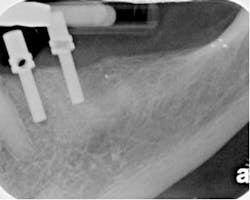
Fig. 1: The initial appearance of the clinical case described. At the time of the clinical examination in my office, the patient was asymptomatic. Percussion, palpation, mobility, and probings were all within normal limits. The tooth had been sealed with a temporary filling after the second visit. From the radiograph, it appeared that the tooth had one conical root with one canal located and shaped. A periapical lesion appeared to be developing at the apex of No. 18. The tooth was restorable. Radiographically, the canal was continuous from the orifice to the apex. The apex was open, patent, and negotiable. The patient’s opening was limited. Access to the tooth was poor. Consent for treatment was obtained. The procedure, alternatives, and risks were explained to the patient and questions were answered. Part of the consent for treatment focused on root anatomy. A single conical root on a lower second molar poses a long-term vertical root fracture risk from a number of different sources including bruxism. In any event, evaluating this case before starting revealed several challenges and considerations:
- The limited opening reduced the vertical space available for rotary nickel titanium (RNT) instruments to shape the canals.
- With another clinician having been into the tooth twice, the possibility of apical transportation and perforation was considered. Clinically, this meant that the risk of master cone and sealer extrusion upon downpack was significant.
- The working length needed determination ideally before the final canal shaping was completed. From the initial radiograph, it was not clear what the estimated working length was (in essence, was this tooth 17 mm or 20 mm?). Rather than immediately putting a RNT file down the tooth and exacerbating a possible apical perforation, it was important to first determine the true working length and then perform the final shaping. A second canal was deemed highly unlikely.
Fig. 2: The completion of the clinical treatment after the use of the Twisted File and RealSeal master cone obturation via SystemB and the Elements Obturation Unit (SybronEndo, Orange, Calif.).Cone fit with tugback is essential and especially so in this clinical case. A .06/20 RealSeal cone was trimmed 5 mm back to create a #50 ISO tip size at its tip. The .06/20 RealSeal master cone is .26 mm 1 mm back, .32 mm 2 mm back, .38 mm 3 mm back, .44 mm 4 mm back, and .50 mm 5 mm back from its tip. Once the cone was trimmed as above, it fit with tugback at the minor constriction (MC) of the apical foramen. Tugback in this context means that the cone resists coronal displacement when a gentle upward force was placed upon it. The master cone in this case was fit to the MC and not withdrawn ½ mm or 1 mm for “safety.” As an aside, if the apical preparation and cone fit are correct, excessive amounts of sealer and obturation material should not be extruded as a result of a SystemB technique or any of the warm vertical obturation techniques. A RealSeal 1 Bonded Obturator™ (SybronEndo, Orange, Calif.) could have been used in this clinical case in lieu of a RealSeal master cone. Its use would have been predicated on an accurate determination of the correct obturator size, correct vertical placement of the obturator in the canal, and keeping the MC at its original position and size. After the obturation, the coronal buildup was placed under the rubber dam and SOM with Maxcem Elite™ (Kerr, Orange, Calif.). The tooth was “rough prepped” for the new crown and the occlusion reduced. A post was not placed in this tooth in favor of placing Maxcem Elite into the orifice. The patient was referred back to his general dentist for crown placement. Conclusions, summary, and observations
- The tooth should have been completed in one visit. There was no indication for the two visits that stretched into a third in this case. Given the fact that the tooth was vital, irreversibly inflamed and the patient without swelling, this clinical case was indicated for one visit treatment.
- The use of formocresol was entirely unnecessary and contraindicated. Had the tooth been treated in one visit, an interappointment medication would have been irrelevant. In the unusual clinical case where a vital tooth requires two visits (for an arbitrarily imposed reason determined by the clinician), either no medication is required (assuming that a pulpotomy or pulpectomy was performed) or calcium hydroxide could be used.
- Accurately determining the position of the MC was critical in the completion of this tooth as it was referred. Incorrect true working length determination (given how open and straight the canal is) could easily have transported the apex and lead to a significant extrusion of filling materials.
Richard E. Mounce, DDS, is the author of the nonfiction book "Dead Stuck" — “one man's stories of adventure, parenting, and marriage told without heaping platitudes of political correctness.” Pacific Sky Publishing. DeadStuck.com. Dr. Mounce lectures globally and is widely published. He is in private practice in endodontics in Vancouver, Wash. Contact him at [email protected].