Focus on Inflammation: The Latest Risk Factor
In recent years, much attention has been placed on evaluating risk factors that make people susceptible to myriad systemic conditions. These include diabetes, cardiovascular disease, respiratory disease, and pregnancy outcomes. Risk factors that are continually being evaluated are smoking, high blood pressure, high cholesterol levels, stress, heredity, age, physical inactivity, obesity, and inflammation. We now have a great deal of information in dentistry about the role of chronic inflammation and the changes it can produce systemically and in the oral cavity. Advances in our understanding of the pathogenesis of a variety of chronic diseases have led to an enhanced appreciation of the significant interactions and associations that occur between oral diseases, and more particularly between periodontal infections and systemic diseases. Analysis of the various means in which periodontal infections and inflammation may influence systemic conditions has been termed periodontal medicine.
Acute and chronic inflammation
In general, inflammation is a localized, protective response of the body to an injury or infection. Characteristically, the clinical signs of inflammation are heat, redness, swelling, pain, and loss of function. It is during this inflammatory response that cells and the chemicals they secrete attempt to dilute, wall off, or destroy the agent(s) causing the injury. A sequence of biochemical events occur which cause the blood vessels to dilate and become more permeable. This results in the activation of the complement, clotting, and kinin systems. If inflammation continues for a prolonged period of time, it may produce problematic consequences for localized tissue as well as the entire body.
Periodontal diseases
Periodontal diseases are polymicrobial-induced inflammatory diseases. They vary from mild gingival inflammation to severe destruction of the periodontium.
Periodontal diseases are among the most prevalent diseases in the world, with gingivitis present in greater than 70 percent and periodontitis in greater than 40 percent of the world’s population, quite likely an underestimate of the true disease prevalence.1
Periodontal diseases are caused by bacteria. Among the 500 or more organisms that populate the oral biofilm (dental plaque), about a dozen pathogenic strains have been identified as being associated with periodontal tissues.2 If plaque is not removed in a timely manner, it undergoes a process of maturation. This results in a more pathogenic state as there is a shift in the bacterial balance toward a more Gram-negative anaerobic bacterial population.
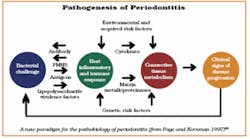
The periodontium responds to the tooth-borne biofilm by the process of inflammation. The bacteria within the dental biofilms release a variety of biologically active products, such as bacterial lipopolysaccharides (endotoxins), chemotactic peptides, protein toxins, and organic acids. These molecules stimulate the host to produce a variety of inflammatory mediators, among them the increased production and release of potent infection-fighting agents known as cytokines. These include interleukin-l-β, interleukin-4, prostaglandins, and tumor necrosis factor-α.3 Ordinarily, cytokines are important for healing. In excess, however, they can cause inflammation and severe damage by overproducing and activating enzymes such as collegenase, which breaks down proteins. They can also stimulate the formation of osteoclasts to resorb bone.
Periodontitis and systemic diseases
It is now thought that these products and responses from the host may influence a variety of important disease pathways, including cardiovascular diseases, diabetes, respiratory disease, or premature parturition. Consequently, investigations are currently directed toward identifying the possible biological pathways by which periodontal infections may influence these disease processes.
Cardiovascular disease (CVD) accounts for 29 percent of deaths worldwide and ranks as the second leading cause of death after infectious and parasitic diseases Atherosclerosis, which is a major component of CVD, affects one of four persons with 39 percent of deaths attributed to it.5 However, despite efforts to prevent the known modifiable risk factors, mortality rates from CVD have remained unchanged throughout the past decade in developed countries. As a result, there has been a renewed interest in a link between CVD and poorly defined environmental exposures such as infectious agents.6 Infectious agents that are currently under investigation include cytomegalovirus, herpes simplex virus, Chlamydia pneumoniae, Helicobacter pylori, and periodontal disease pathogens. Epidemiologic studies in human populations indicate a modest but consistent (1.3-2 fold) increase in the risk of CVD among people with periodontitis.7 Patients with periodontal disease share many of the same characteristics as patients with CVD, including being predominantly men, older, of a lower socioeconomic status, stressed, smokers, and diabetic.8 It has also been found that many patients with periodontal disease also have CVD. These observations have suggested that periodontal disease and atherosclerosis may share similar or common etiologic pathways. Periodontal infections with their known high prevalence may contribute significantly to the proposed infection-related etiology of CVD.9
Recent evidence indicates that the inflammatory response is the common element. This is an overreaction of the immune system that causes injury to tissues in the body. A common link between patients with both heart conditions and periodontal disease may be elevated levels of C-reactive protein (CRP), a marker for the inflammatory response. Some believe that immune factors causing this response are released into the blood stream during periodontal disease and then cause injury in the arteries supplying blood to the heart. Evidence also suggests that the bacteria, particularly P. gingivalis, may play a direct role in arterial injury. It is now believed that there is no actual causal relationship, but that common factors induce inflammation and damage resulting in diseases in the blood vessels and in the periodontal environment.10 A recent consensus report published by the American Academy of Periodontology11 acknowledges the strength and consistency of the association between periodontal disease and cardiovascular disease.
Diabetes and periodontal diseases
Two common chronic conditions - diabetes and periodontal disease - have a complex connection that goes in both directions. While it has been established that people with diabetes, a risk factor for periodontitis, are more prone to developing periodontal disease, there is new research suggesting that periodontal disease may, in turn, be a risk factor for diabetes. Some evidence has suggested that the bacteria causing periodontal disease may enter the blood stream and activate immune cells. These activated cells produce inflammatory cytokines that have a destructive effect throughout the entire body. In the pancreas, the cells responsible for insulin production can be damaged or destroyed by the chronic high levels of cytokines. Once this happens, it may induce Type 2 diabetes, even in otherwise healthy individuals with no other risk factors for diabetes.12
Pregnancy
The bacterial infections that cause moderate to severe periodontal disease in pregnant women may also increase the risk of premature delivery and low-birth-weight infants. Preterm delivery estimates are at 6 to 15 percent of all live births, according to The Oral Care Report (Vol. 14, No. 4, 2004). Research indicates that the bacteria from periodontal disease or their products (endotoxins) may trigger the same factors in the immune system as genital and urinary tract infections. Specifically, the biologic substances called prostaglandins and tumor necrosis factor produce inflammation in the cervix and uterus that can cause premature dilation and contractions.13 For this to be minimized, it is recommended that women have a periodontal examination before becoming pregnant or as soon as possible thereafter.
Respiratory
Clinical trials aimed at documenting the association between periodontitis and respiratory diseases may be more difficult due to the shared risk factors, especially smoking, that may mask other important factors in the etiology of disease progression. Smoking in both cases is known to suppress the immune response and compromise the inflammatory response.14 However, studies have shown that bacteria which reproduce in the mouth can also be carried into the airways of throat and lungs, increasing the risks for respiratory diseases and worsening chronic lung conditions, such as emphysema.15
Future strategies
Because oral diseases in general are treatable and usually not life-threatening, they have erroneously been perceived as having little relationship to other aspects of health. However, oral health and systemic health are closely related. There is a strong correlation between deterioration of oral health and deterioration of general health. This is primarily due to the fact that several oral diseases and noncommunicable chronic diseases have common risk factors such as inflammation. Although definitive cause and effect have not been established, recent research findings indicate that some association exists between different systemic conditions and oral health. These have been presented via different mechanisms which have demonstrably supported these associations. If a periodontal/systemic link is further studied and validated in intervention trials, dentists and dental hygienists will then be able to participate to a larger extent in promoting general health to patients, screening those at high risk for both conditions, and providing periodontal treatments targeted at reducing inflammation and improving overall health. For now, clinicians need to know the strengths and limitations of the available evidence as they diagnose and treat patients with periodontal disease. By realizing that oral health is a critically important component of general health, we, as practitioners, are also ensuring that it has a significant impact on the quality of life.
References
1 Albandar JM, Brunelle JA, Kingman A. Destructive periodontal disease in adults 30 years of age and older in the United States, 1988-1994. J. Periodontol 1999; 70:351.
2 Genco RJ. Periodontal risk factors: clinical implications. J. Periodontol 2003; 74:1092-1093.
3 Scannapieco FA. Periodontal inflammation: from gingivitis to systemic disease? Compend Cont Educ Dent July 2004; 25(7 Suppl 1):16-25.
4 The World Health Report 1997 - conquering suffering, enriching humanity. World Health forum. 1997; 18:248-260.
5 American Heart Association. Heart disease and stroke statistics - 2004 Update. Dallas, Texas, American Health Association, 2003.
6 O’Connor S, Taylor C, Campbell LA, et al. Potential infectious etiologies of atherosclerosis: a multifactorial perspective. Emerg Infect Dis 2001; 7:780-788.
7 Paquette DW. The periodontal-cardiovascular link. Compend Cont Educ Dent Sept. 2004; 25:681-692.
8 Beck JD, Offenbacher S, Williams R, et al. Periodontitis: a risk factor for coronary heart disease? Ann Periodontol 1998; 3:127-141.
9 Umino M, Nagao M. Systemic diseases in elderly dental patients. Int Dent J 1993; 43:213-218.
10 Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA 1998; 279:1477-1482.
11 Scannapieco FA, Bush RB, Paju S. Associations between periodontal disease and risk for atherosclerosis, cardiovascular disease, and stroke. A systematic review. Ann Periodontol 2003; 8:38-53.
12 Soskolne WA, Klinger A. The relationship between periodontal diseases and diabetes: an overview. Ann Periodontol 2001; 6:91-98.
13 Goldenberg RL, Hauth JC, Andrew WW. Intrauterine infection and preterm delivery. N Engl J Med 2000; 342:1500-1507.
14 Page RC. Periodontitis and respiratory diseases: discussion, conclusions, and recommendations. Ann Periodontol 2001; 6:87-90.
15 Scannapieco FA, Wang B, Shiau HJ. Oral bacteria and respiratory infection: effects on respiratory pathogen adhesion and epithelial cell proinflammatory cytokine production. Ann Periodontol 2001; 6:78-86.
16 Page R, Kornman K. The pathogenesis of human periodontitis: an introduction. Periodontol 2000 1997; 14:9-11. ■
Patricia Sukmonowski, BSc, DDS
Dr. Sukmonowski, a periodontist, maintains a private practice in New York City, limited to periodontics and implant dentistry. A diplomate of the American Board of Periodontology, she is also an assistant clinical professor of periodontics at New York University College of Dentistry. You may contact her at [email protected].