Are you frustrated with the fit of contacts on lab restorations in your practice? You are not alone!
As Dental Technical Support Manager at Whip Mix, I’ve received several calls in the last few weeks from both laboratory personnel and dentists regarding the fit of contacts on laboratory restorations when they’re returned to the doctor for placement. Most have been loose contacts and some have been tight, but either way the situation is frustrating for the laboratory, the dentist, the clinical staff, and the patient.
Generally the dentists call to see how they can get their laboratory to improve the model work being done, and they’re sure that it involves the expansion of the stone. After many years of working with hundreds of dentists, I can tell you from experience that the No. 1 reason for contact issues is temporaries. The second is distorted impressions, and the third is a laboratory process that I will explain here.
We can all agree that teeth move (otherwise orthodontia is a scam!), and they move differently on different patients. When teeth move is a variable based on a lot of things, but the one we’re talking about here is the pressure or lack of pressure that temporaries place on the teeth adjacent to a preparation. The “tightness” of the temp in the now-prepped space can place enough pressure or lack of pressure on the teeth to move them slightly out or collapse them in from the original position captured in the impression sent to the lab. The contacts of the crown returned for placement will reflect the position of the teeth as they were captured in the impression two weeks earlier. Thus the clinical staff placing the returned restoration may see a difference in how the crown fits and how the temporary fits. That is, if the temporary is still in place at the seat date.
To help the lab understand the individual clinical method employed for checking these contacts, it would be wise for the dentist to invite the lab staff to sit with the clinical staff as they place a temporary. In so doing they can feel the “snap” of the floss or the “pull” of the shim stock desired by the clinician, and then repeat that in the laboratory. If the temp is too tight, they can also help the staff understand why this is problematic.
This also applies for the occlusal contacts. When the dentist calls and says “a crown is too high,” and the lab knows that they took the crown out of occlusion on the models by two to three occlusal tape thicknesses (19-88 µ), we know that either the preparation or the opposing dentition has erupted. Again, the most likely factor to cause this is the temporary.
I’ve personally had crowns placed, and the extended function assistant simply asked, “How does that feel?” marked with paper or film, and then wholesale ground away until I said I couldn’t feel interference. Remember, I was still partially numb. As a technologist I focused on the touch and feel of the other teeth in the quadrant. But what about most people, who know nothing about occlusion? It’s not good enough to just not interfere. Temporaries need to be placed correctly, and they need to reflect occlusion that was there originally to hold the correct space, and duplicate anatomical factors sent in the impression to the laboratory.
ALSO BY CRAIG PICKETT:
What 3 factors in dental labs affect consistency in casting during investment process?
Clearing the fog of digital dentistry
The common errors in model work on the lab side are twofold – first is the addition of water to gypsum that is already mixed as the gypsum is starting to set. This can cause changes to the expansion of the next models poured and should not be done. The simple addition of a little less or a little more water at the beginning does not affect expansion. However, it does affect all of the other parameters of the stone.
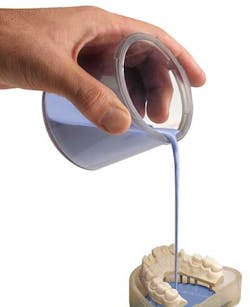
Second and most important is the relationship of the base stone to the die stone master model. In the process the die stone is fully set and pinned, and then the base stone is poured to secure the pins. If the lab does not wait long enough for the base stone to set and expand before separating the dies, this error will allow the base stone to pull apart the now-individual pieces of the master model and change the relationship. The best combination is to always use a low expansion basing stone (.08%-.10% at two hours). Regardless of the expansion of the die stone, wait at least two hours before separation unless the stone has specifically been designed for rapid use and achieves a minimum of 85% expansion in the first hour. If the lab is using a plastic base, then the same principle of time should be applied to the die stone prior to separation of the dies.
The issue of tight or loose contacts needs to be examined by both the clinical and laboratory sides, and a solution, not an adjustment of the crown, needs to be found so that patients receive the best and most consistent dentistry possible.