Caries detection
Are you still looking for holes?
By Wendy Negron, RDH, MS
We have all heard the resounding mantra of the big change in dentistry from the surgical model to the medical model. As a whole, the profession is slowly becoming aware of this transition, but many of us are not clear on how and when to begin making this change in our practices. Just like any other discipline in medicine, early detection of disease is critical. We have been treating caries with all of the tools available to us and we discuss prevention of this disease with our patients, but it is usually an uphill battle and all too often surgery - the drill - is our only option.
Until recently, caries detection methods remained unchanged for the past 50 to 100 years. The most commonly used detection methods (visual and/or tactile examination and radiographs) focus on the end point of the caries disease and are necessary for a thorough diagnosis, but each have limitations. One produces radiation for us as well as the patients, one can destroy the surface mineral of small lesions that could have been remineralized, and all can be affected by irregularities that can make accurate detection problematic.
For many years, caries was viewed as a condition rather than a process or a disease. Over the past several years however, more has become known about the caries disease process and the conditions needed to create the cavitated lesion. We now know that caries is an infectious bacterial disease that can be spread from person to person by physical contact. We also know that there are specific bacteria that cause the disease, and that certain medications can prevent the bacteria from spreading. We know so much information, yet we find it difficult to change our practicing habits. The drill continues to win the battle. It’s like having a fire in a house without a smoke detector. Chances are good that by the time the fire department arrives, the damage is already done.
Visual examination
Visual examination is the first and fastest technique used to detect decay. This technique relies on the idea that, as decay progresses, the tooth structure changes color. The normal glossy sheen of tooth enamel becomes clouded, loses luster, and appears chalky white. This detection method is sensitive enough to detect decay once it has become a white spot. While white spots can sometimes be remineralized, the lesion may have already done significant damage to the enamel and may have progressed into or near dentin.
Visual examination is used on all surfaces that can be seen with the naked eye, however it lacks the ability to see interproximal areas. These areas can only be seen when the adjacent tooth is removed or missing or when the decay has progressed enough that it wraps around the facial and lingual surfaces of the tooth.
There are aids to visual detection in the form of disclosing dyes and transillumination. Dyes use a strong color differential to show porous surface sites on an otherwise sound tooth, while transillumination uses the scattering of light to show areas that are lacking mineral. Both techniques assist visual examination in finding more diseased sites, but are only as sensitive as the naked eye.
Tactile examination
Tactile examination is another method of detecting decay on the tooth surface. This technique focuses on, but is not limited to, occlusal pits and fissures that create difficult conditions for visual decay detection. The variations in the tooth surface create reflections, light spots, dark spots, and contain stains. These “interferences” create problems when visually trying to discern decay from stains or other common static. The use of a dental explorer adds a new dynamic to the process.
Demineralization changes the mineral content of a tooth surface. Both dentin and enamel dissolve readily under the proper acidic conditions. Enamel is more dense in mineral content than dentin and therefore dissolves much slower. Enamel begins to dissolve when it is subjected to pH below 5.5 for a period of time. Dentin begins to dissolve at a pH near 5.9. As the mineral content changes, the structure of the tooth becomes less sound and more prone to collapsing and breaking from pressure.
Imagine a table with six legs that is supporting a 500-lb. weight. If you remove one leg, the table has less support. If you continue to remove legs from the table, eventually the 500-lb weight will crush the table. The dental explorer can be the equivalent of a 500-lb. weight on the surface of a tooth. If there is a demineralized area, the pressure of the explorer will puncture the lesion and the instrument will “stick” on the tooth. Once this has taken place, remineralizaton can no longer occur. This site must now be restored.
Radiographs
Radiographs (X-rays) are the third method of detection. This method added a facet that was missing in the caries detection process. X-rays work by passing radiation through the tissues of the face and mouth and onto a sensor plate or X-ray film. The film is then developed and differences in densities of structures can be seen. Harder substances such as tooth enamel show up as white areas, while less dense areas show up as black or transparent areas.
Unfortunately, the limitations of radiographs include the inability to see around or even near a filling or crown, lack of sensitivity of the system to detect decay, and the radiation emission for the patient and office staff. Blackout zones surrounding restorations may also leave you guessing as to what is actually there. Have you been able to see early secondary decay on a radiograph? What about a white spot? Some white spots are hard to see with the naked eye, and all but impossible with radiographs. Most important of all, lesions on radiographs tend to show up at about 200-300 microns into the tooth. Restorative procedures at this depth are almost always required.
New, digital radiographs require much lower concentrations of radiation to capture an image and the sensitivity of radiographs is improving with the addition of computers, but they are still confirming the need for invasive procedures.
Light fluorescence technologies
There are two systems available that use light fluorescence to detect caries activity. However, there are substantial differences between them. One system, DIAGNOdent from KaVo®, uses a red light source to detect metabolic waste from bacteria that are present in the body of the lesion. This can be a good indicator of a problem area. However, it is important to have a very clean surface before DIAGNOdent is used because metabolites on the surface of the tooth will create detectable fluorescence as well. This can skew the results. DIAGNOdent provides numeric values based on the specific placement of the light tip. As the tip moves along the tooth surface, the values change based on the amount of metabolic waste. Values also change based on the location and angle of the tip in relation to the tooth surface. This system can be useful as an aid in caries detection, but must be used carefully to avoid false positives.
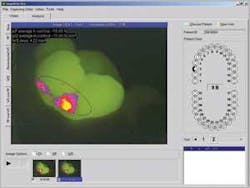
The newest diagnostic tool that uses light fluorescence technology is the Inspektor™ Pro system, developed by Inspektor Dental Care of Amsterdam and available in the United States from OMNII Oral Pharmaceuticals. The system has been shown to detect up to 10 times more early lesions (pre-cavitation) than traditional methods. Inspektor Pro uses Quantitative Light-Induced Fluorescence Technologies, or QLF, comprised of a specific blue light and proprietary software. Like the DIAGNOdent system, Inspektor Pro detects bacterial activity. However, the similarities end there. This new system is very different from DIAGNOdent in that it also measures the mineral content of the tooth. Mineral loss (demineralization) is quantified by the system based on the differences in fluorescence of sound and compromised surfaces. The Inspektor Pro software analyzes the loss or gain of fluorescence and “maps” the entire area in question, quantifying the varying levels of demineralization around the site. The system also allows clinicians to accurately capture the same image during successive office visits to track changes in demineralization and remineralization. Identifying caries at this very early stage and having the ability to quantifiably track the effects of preventive strategies provide clinicians with information that has never before been available. The computer-generated map also is excellent for patient education and motivation. Use of the Inspektor Pro will add time to an office visit and may require a different approach to traditional scheduling. Nevertheless, the images can be taken by a trained auxiliary and interpreted by a clinician.
The Inspektor Pro system costs around $24,000. As with many new treatment options, insurance reimbursement is not automatic. How will offices re-coup their investment? The first step is telling the patient that you, the medical professional, recommend the procedure and that it might help them avoid surgery! Some practitioners may decide to include the Inspektor Pro procedure as part of their Periodic and/or Comprehensive Oral Examinations (CDT codes 5010 and 5020 anticipate the use of new diagnostic tools.), raise their fee accordingly, and advise patients that insurance may or may not cover the entire cost of the exam. Other offices may choose to offer the procedure as an optional advanced diagnostic tool. This approach is common in many areas of medicine.
The future of caries detection is bright
Will any of these methods eliminate the need for restorations in the dental office? It’s not likely. There will always be patients who avoid the dental office until it is too late. As people live longer and keep their teeth longer, even the best oral care may not be enough. Of course, heredity, dietary habits, and the use of many prescription medications also can contribute to poor oral health.
Visual examination, tactile examination, radiographs, and light fluorescence all have their place in the diagnosis and treatment of caries. Light fluorescence is the newest method for detection. Allowing dental professionals to easily see the earliest signs of demineralization represents a significant advancement in the treatment of caries. Is it a new way of treating caries? Yes. Will it require a change in our approach? Yes. Just like the CT scan and MRI have done for internal medicine, light fluorescence changes the way we can detect and treat the caries disease. How many of your patients would refuse a CT scan if their internist told them it was needed? We are making great strides in detecting the caries disease earlier, when medications and/or changes in oral care can prevent or reverse the disease process. That’s good news for everyone.
Wendy Negron, RDH, MS is the manager of Clinical and Professional Relations for OMNII Oral Pharmaceuticals. Ms. Negron is responsible for assessing, testing, and evaluating new products from a clinical hygiene perspective. She works closely with clinicians to provide the latest information about treatment protocols and medications in the preventive care arena. Reach her at (800) 455-3386, ext. 1421 or e-mail [email protected].