The missing factor in cosmetic dentistry - occlusion
By Michael Teitelbaum, DMD, FAGD
Imagine your best day ever in the office. Picture finishing work on your favorite patient. What did the work look like? Was it easy or almost predictable how perfect it would be? Were there good feelings all around? Were you proud of completing a job well done? How about payment? Was everyone satisfied with a fair fee for excellent service? Wouldn’t it be great if not only our favorite patients could be like this, but every patient, every single day? All these positives rarely happen by accident; in general, they all require advance planning of a specified goal and the underlying knowledge to accomplish it. Most dentists graduate dental school: a) traumatized, and b) with the ability to churn out amalgams. Some dentists aspire to more - to minimize or eliminate amalgams, to do fixed prosthodontics, tooth-colored restorations, cosmetic dentistry, etc. - but are turned back by insufficient time, inability to get paid superior fees for superior service, and/or fear of breakage.
Things break because they are overloaded by stress. In the mouth, form follows function or, in other words, stress is caused by factors of occlusion. Conversely, in our practices, things breaking can cause mental overload and stress. If our goal is to minimize stress in both our practices and our dentistry, then a thorough understanding of what causes those stresses and a plan to eliminate them is in order. Thus, by understanding fundamental factors of occlusion, we can increase the life span of our restorations, expand the range of services we offer and improve our financial conditions, as well as our personal and professional satisfaction.
Occlusal considerations
There are four major factors in occlusion:
- Simultaneous, pinpoint contact in centric
- Immediate anterior disclusion in all excursions
- Progressive anterior guidance
- Narrow Buccal-Lingual occlusal width
These basic generalizations on the surface may not appear to cover every situation, yet when considered closely are quite powerful.
Simultaneous, pinpoint, contact in centric - In stating that all teeth must contact, this can immediately rule out many styles of occlusion, including most forms of bilateral balance. Further, simultaneous contact assures that forces of occlusion are evenly distributed along all teeth. Pinpoint contact is important because it has been shown that most eccentric interferences happen in an area of 0.3 mm in and around centric. The term centric itself implies a repeatable occlusal position and there are many locations, definitions, and types. The choice must be made by each restorative doctor for each individual case, and further discussion of the pros and cons of the various concepts of centric is well beyond the scope of this article.
Immediate anterior disclusion in all excursions - Continuing in our model of occlusion, we proceed from our starting point of centric into excursions. Immediately, all posterior teeth are disoccluded by the anterior teeth. In other words, although all teeth are touching in centric, the immediate lift off - guided by the anterior teeth - prevents the posterior teeth from touching anywhere other than centric.
Progressive anterior guidance - The most commonly known form of anterior guidance is canine guidance. This is an excellent starting point, but why should all excursive forces be concentrated on one poor canine? Instead, by designing a progressive anterior guidance, it is possible to spread out excursive forces equally so they are distributed among all of the anterior teeth. Therefore, although we begin with canine guidance, the guidance should quickly and gently transfer to the lateral incisors, then to the central incisors upon which to ride the rest of the lateral excursion, all on a pinpoint-sized contact.
Narrow buccal-lingual occlusal width - This concept mostly relates to lab-fabricated dentition. It is important to remember that although they may be quite skilled, lab technicians are not doctors; they are technicians. As craftsmen, lab techs enjoy fabricating porcelain, so much so, in fact, that many times they will fabricate a crown and actually make it larger than the tooth it was replacing. This over-building can result in unsupported porcelain - which is more prone to fracture - and extra-wide buccal and lingual cusps with porcelain sticking out, presenting the possibility of the jaw finding eccentric balancing contacts. This can lead to bruxism.
Occlusal anatomy
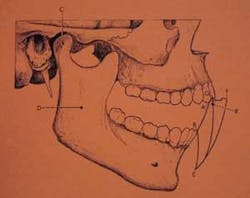
To impress dentists with their skills, lab technicians will routinely decorate the occlusal surface of restorations with a myriad of unnecessary stains and grooves, also known as “cat scratches.” These embellishments, although admired by dentists ignorant of their pointlessness, are many times offensive to patients. The posterior occlusal anatomy truly necessary from a gnathologic standpoint is quite simple, and consists of the “escape grooves” needed to allow opposing cusps to travel through fossae in excursions without hitting, throughout the envelope of motion. The envelope of motion is most popularly thought of in the sagittal plane, as in figure 1; it can also be viewed from the occlusal plane as seen in figure 2.
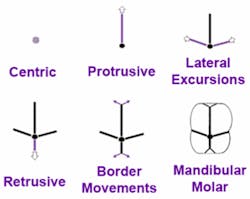
Another way to think of it is to reconsider our four major occlusal considerations. We know from the first one listed - simultaneous, pinpoint contact in centric - that all that is needed in centric is a pinpoint contact with an opposing cusp in a central fossa, as in figure 3. We then can imagine this opposing cusp traveling into protrusive and the path it would trace, as in figure 4. Returning to centric, we can further picture our opposing cusp traveling into right and left lateral excursions, as in figure 5. Even in classic centric relation, one must always allow for a small amount of potential retrusive movement, as seen in figure 6. Finally, the mandible can make minor border movements, as seen in figure 7. It’s no coincidence, then, that if we superimpose these movements onto the occlusal of a mandibular first molar, they perfectly match the basic necessary dental anatomy (figure 8).
null
Mechanical considerations
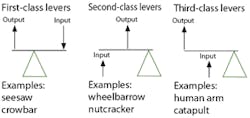
The importance of these escape grooves is to eliminate the possibility of posterior eccentric interferences, and minimize the occlusal forces on anterior teeth. Imagine trying to cut something hard or thick with a pair of scissors. Empirically, you know to gain more force you would not use the tip of the scissors, but cut closer to the handle, or fulcrum. In point of fact, this changes the mechanical advantage from a Class 3 lever system to a Class 2 lever system (see figure 9), and generates a tremendously greater amount of force. But what if you could have something contact the outer tip at the same time as close to the fulcrum? All the force from the fulcrum would be transmitted to the tip.
It’s the same with the mandible - more force is generated closer to the fulcrum or condyle. If there are balancing contacts or interferences, force is transmitted from the posterior teeth - which are designed to handle it - to the anteriors - which are not. This causes many of the fractures and chips we see in anterior teeth, and is a critical factor in restoring them.
Clinical considerations
Figure 10 shows just such a fracture of an anterior tooth. In this simple example, we can see there currently are no posterior balancing contacts and the damage was probably done from a long-term anterior balancing contact in crossover position between teeth Nos. 9 and 25 (figure 11). This balancing position most likely began when there actually were posterior teeth balancing against these two teeth. These posterior balancing teeth have most likely been either extracted or exfoliated. Since this patient had long since felt that his maxillary central incisors were too long anyway, it was a relatively simple procedure to shorten them to eliminate the fractured area (figure 12), then round and polish the incisal edges of both maxillary and mandibular incisors to eliminate any future potential balancing areas. Figure 13 shows the patient having slid all the way to a maximum lateral excursion, finding no area upon which to balance.
Our next case shows a young woman who presented having just fractured teeth Nos. 9 and 8 (figure 14). Sliding her mandible into extreme excursions finds her jaw naturally stops when tooth No. 20 “clicks” into the fractured area, as in figure 15. Upon further examination, it can also be seen that she has posterior balancing contacts at the same lateral crossover position on both right and left (figures 16 and 17). This balancing tripod effect most likely contributed to excessive force long-term on the anterior teeth that, unable to take the load, eventually fractured. There is no composite material stronger than enamel - the hardest substance in the human body. Her balancing contacts enabled the patient to develop enough force to fracture enamel, so it is only reasonable to assume that she would be able to fracture any composite replacement in a much shorter period of time.
Initial attempts, therefore, were to eliminate the posterior contacts in the locking crossover position. Unfortunately, this only shortened her vertical dimension in this position, deepening the anterior overlap into the fracture. The only way to eliminate excessive forces caused by the posterior contacts was to build up the fractured incisal edges, creating an anterior guidance with a Class 3 lever system.
After selecting a shade, Nos. 9 and 8 were beveled (separately), then sandblasted, etched, and bonded with a hydrophilic bonding system. They were then incrementally built up and cured with matching shaded composites until the posterior cusps were no longer contacting in the crossover position. The patient’s ability to smoothly translate throughout all excursions without locking was verified and then double-checked with 40-micron thick articulating paper. Both anterior and posterior teeth were then highly polished. Upon examination, the patient remarked that her newly restored teeth looked just as they had when she was younger - before she’d begun to wear them down.
Financial considerations
It is important to understand how mechanical forces affect occlusion throughout the envelope of function and in all aspects of restorative dentistry. In the cases shown here, it was critical to first understand the cause of the problems before attempting to fix them. Had the teeth in question been repaired without regard to the occlusal forces that had caused the fractures, there is no question that the repairs would have been short-lasting. Unfortunately, this kind of diagnosis and meticulous treatment requires substantially more time throughout all phases of treatment. Spending more time per patient obviously translates into not being able to physically treat as many patients. While it certainly should be our mission to help all in need, unless we are fairly compensated for this increased time and subsequent drop in patient flow, it can lead to financial difficulties and an inability to help anyone. It is unlikely that a dentist doing this kind of thorough occlusal/restorative treatment could long survive accepting merely a few dollars per restoration as offered by many managed care plans - especially when just overhead would likely come to a high multiple of this number. Is it fair to ask our patients to pay a higher fee for a higher quality of service? As providers of dental care services, should we model ourselves after Nordstrom or Wal-Mart? The Four Seasons or Holiday Inn? This is a question that each dentist must answer individually. Just as there must be room in the marketplace for the comprehensive, Pankey-style, occlusally oriented, amalgam-free, all-bonded, insurance-independent practice, so must there also be room for the opposite. In a free marketplace, one cannot exist without the other. Our choice is to decide which we can be, which we want to be, and if we can live with that decision.
Editor’s Note: References available upon request. This is the first of a yearlong series of articles from the American Academy of Cosmetic Dentistry (AACD). The AACD and Dental Equipment & Materials are working together to provide articles that will help your practice. For more information about the AACD, log on to www.aacd.com or call (800) 543-9220.
Dr. Michael Teitelbaum is a Clinical Research Associates evaluator who taught for eight years at NYU College of Dentistry. He lectures across the U.S. on various topics in cosmetic dentistry and is available to lecture for you as well. He is the author of numerous articles in professional publications, and has a mostly cosmetic practice in Briarcliff Manor, N.Y. He can be reached at [email protected], or by mail at 1312 Pleasantville Rd., Briarcliff Manor, NY 10510.