Predictable impressioning
By John C. Cranham, DDS, Chesapeake, Va.
Within a well-run dental practice, a direct relationship exists between predictability and positive trends. These benefits include increased production, decreased overhead, increased profitability, decreased stress, and increased happiness of the entire dental team. The better we become at doing procedures correct the first time, the more we can experience the attributes previously mentioned. Becoming predictable in our work should be the primary focus of every dental practice. Without predictability, there is great uncertainty, and found within uncertainty is a high degree of stress.
For a dental practice that does any amount of indirect restorative dentistry, learning a tried-and-true technique that consistently captures the necessary details of an impression is a vital component. Yet, after speaking to hundreds of laboratory owners over the last several years, it is obvious that consistently excellent impressions are a rarity.
Start with healthy tissue
It is important to understand that, in fabricating an indirect restoration, the purpose of the impression is not to simply capture the details of the hard tissues. The goal is to also capture the stable relationship of the gingival tissues. If we do indirect restorative procedures in the presence of gingival inflammation, the final restorative result will likely be inadequate, no matter how "good" the impression. After final crown placement, when the gingival tissues return to normal size, shape, and contour, exposure of a margin will occur. While the crown may fit fine, the outcome is likely to be below the patient's esthetic expectations.
Beginning with healthy tissues will also simplify the impression-making process. Bleeding tissues can be controlled, but should not be "the norm." Taking patients through proper periodontal procedures and completing all necessary preliminary mouth preparation will add tremendous predictability to all indirect esthetic/restorative dental procedures.
Soft-tissue management
From time to time, it is necessary to control a minor amount of gingival bleeding during a restorative procedure. Inadvertently nicking the tissues during margin refinement does occur occasionally and it is essential to have the ability to quickly control hemostasis. Viscostat from Ultradent dispensed from its Dental Infusor is a fast, predictable way to obtain 100 percent control.
Start with an impressable preparation
Most restorative dentists do not trim their own dies. While many teaching institutions recommend doing this, with consistently excellent impressions, it is actually an unnecessary step. It is important, therefore, for dentists to prepare teeth in a way that their margins are easily identifiable. We should learn to prepare teeth with a consistent margin design 360 degrees around the tooth. If a contemporary metal ceramic material is your restorative choice, then a chamfer margin with the same general look should be utilized. If you prefer more of a knife-edge or even a shoulder, the key is to develop a preparation style that your dental laboratory gets used to seeing. You want to avoid having a margin that starts as a chamfer, then turns into a knife-edge, and then ends in a shoulder. These become very difficult to read and trim. Preparing teeth with consistent margin design will add tremendous predictability in the laboratory reproduction of your preparations.
Consistent margin placement
Consistent margin placement is key to providing a restoration that will meet the esthetic goals of the patient and the optimum health of the restorative result. Not preparing far enough into the gingival sulcus will lead to esthetic problems, while going too deep will invade the biologic width.
By beginning with healthy tissue and using normal probing depths, a technique can be employed to consistently place the margin one-half the depth of the healthy pocket. If the pocket is 2.5 mm deep, then the margin should be placed 1.2 mm underneath the tissue. This will create an invisible margin, and one that exists in a healthy relationship within the periodontal structures.
Retraction options
There are many excellent ways to retract tissue if the only goal is to simply expose the gingival margin. Laser troughing and electrosurgical procedures are both excellent ways to expose the restorative margins. A retraction cord, while more time-consuming, can be used to more predictably place the margin in the ideal zone within the gingival sulcus.
A two-cord technique has been described to accomplish this goal. The technique described in this article is a modification of this process utilizing contemporary materials.
- Start with an impressable preparation
A step-by-step approach to an ideal final impression
null
In figure 1 (above), you will see a tooth prepared for a Captek Crown. The preparation has adequate reduction (as described in Part 1 of this series, printed in January) and has been smoothed and polished. The margin design is that of a chamfer, around the entire circumference of the tooth. Employing this type of preparation guideline will dramatically increase the readability of your impressions since your laboratory support will know exactly what it is looking for. Whatever margin design you personally prefer, keeping it consistent will increase the quality and predictability of the final restorative result.
- Control the soft tissue through preliminary mouth preparation and chemotherapeutics
Starting with a healthy mouth is a prerequisite of any restorative procedure. Proper preliminary mouth preparation should include any and all procedures to get the mouth completely free of disease prior to the final restorative phase. Healthy tissue will make our job easier and the final esthetic/restorative result more predictable.
Additionally, chemotherapeutic agents such as Viscostat (Ultradent Products, figure 2, below) can be used by directly applying it to the tissue to stop any localized bleeding. This can also be used to soak the retraction cords (figure 3, below). This chemical agent (Ferric Sulfate), not only rapidly achieves hemostasis, but also fixes the tissue, holding it in the retracted position for a longer period of time. This material is an important component of any restorative dentist's armamentarium.
null
null
Placement of first cord
Prior to final margin placement, the first cord should be packed. A 00 Ultradent cord that has been soaked in Viscostat is placed into the depth of the sulcus (figure 4). As shown in figure 5, the goal is to have it perfectly fit once around the tooth. Pressure should be applied so that the 00 cord is sitting at the base of the healthy pocket.
null
null
Margin refinement
Once the tissue has been retracted with the first cord, the margin is finished by dropping the margin to the top of the cord (figure 6, below). The placement of the cord will protect the biologic width and prevent us from going too far into the pocket. This is where this technique may have an advantage over laser or electrosurgical retraction. While other techniques can rapidly attain exposure of the restorative margin, there is greater risk of invading the biologic width or leaving the postoperative margin visible.
null
Addition of contemporary retraction material
A very popular method of obtaining ideal retraction involves the placement of two cords on top of one another within the pocket. This technique follows a similar path, but uses a contemporary dental material called Expasyl (figure 7, below), recently introduced by Kerr. This material has a clay-like consistency that is released (under pressure) around the gingival sulcus (figure 8, above). It has hemostatic agents within its body and also has the ability to absorb crevicular fluid. The most positive clinical effect observed is not just great retraction, but a very dry field. In fact, there seems to be a complete absence of fluid around the preparation — a quality that makes for an ideal impression.
null
null
Apply pressure with Comprecap
After dispensing the appropriate amount of Expasyl over the retraction cord (figure 9) circumferentially around the tooth, a Comprecap (figure 10) is placed over the prepared tooth. Comprecap, made by Roeko, look like a hollowed-out cotton roll, but are open only on one side and are firmer (figure 11). Once placed over the prepared tooth, the patient can bite on the Comprecap, pushing the Expasyl further into the pocket (figure 12). This provides additional retraction by forcing the tissue further away from the tooth. When you combine this benefit with the additional hemostatic and drying properties of this material, Comprecap makes for a very predictable method for margin capture.
null
null
null
null
Visually inspect retraction objectives
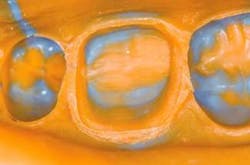
After washing away the Expasyl (simply remove by spraying with a three-way syringe) and removing the retraction cord, visual inspection is the final step before taking the impression. This is when the doctor should put on his or her loupes and, using excellent lighting, visually inspect the retracted tissue (figure 13, below). All margins should be easily viewable with a minimum of .5 mm of additional tooth structure apical to the margin. Figure 13 exhibits the ideal retraction goals.
null
Inject with quality impression material
A polyvinyl impression material such as Take One from Kerr can be utilized to complete the impression procedure. While this material has hydrophilic properties, every effort should be made to keep the field dry. Dry angles, cotton rolls, and suction should be employed to keep saliva out of the field. This is particularly important in the mandibular area. When injecting (figure 14, below), keep the tip angled at the margin and burnish the material around the tooth. The thixatropic nature of this material will allow it to flow upon itself, eliminating voids, bubbles, and fins that can find their way into an otherwise perfect impression.
null
Visually inspect impression
The final step is visual inspection of the impression. Loupes or some sort of magnification should be used to check the details of the master impression. As previously mentioned, all margins should be visible with a minimum of .5 mm apical to the marginal tissues (figure 15).
By combining all of the elements of healthy tissue, correct preparation design, predictable retraction, and highly esthetic porcelain contour and color, we can all achieve excellent clinical results. The outcome can be seen in this delivered IPS d.SIGN Porcelain to Captek restoration (figures 16 and 17).
null
null
Indirect restorative procedures can be a highly predictable, highly profitable component of any dental practice. To achieve this, however, the dental team must employ some simple, disciplined steps to achieve consistent results. This article has outlined a step-by-step, highly predictable method of obtaining an ideal final impression.
Acknowledgment: The author would like to thank the technical staff of Dental Arts Laboratories, Inc. in Peoria, Ill., for their excellent ceramic artistry in preparation of this case. Call (800) 227-4142 to contact DAL.
Note: For complete information on Cranham Dental Seminars, visit www.cranhamdentalseminars.com or contact Dr. John Cranham's office at (757) 465-8900.