Emerging applications for the soft-tissue diode laser
Written by Lori Trost, DMD and Karen Kaiser, RDH
Since the introduction of the first dental diode laser in 1995, numerous diode lasers are now available.1 By 1999, most dental diode laser devices on the market had Food and Drug Administration (FDA) clearances for all minor periodontal and oral surgery procedures, including subgingival curettage. However, not all diode lasers have the same FDA clearance.
The FDA is the federal agency that regulates the distribution and sale of dental devices in the United States.2 It allows manufacturers to market dental devices based on data they submit demonstrating that a product is safe and effective for specific uses. The FDA strictly controls manufacturers' claims for many dental products, but it has no authority over the practice of dentistry. Duties performed by dentists, dental hygienists, and dental assistants are regulated by individual state dental practice acts.
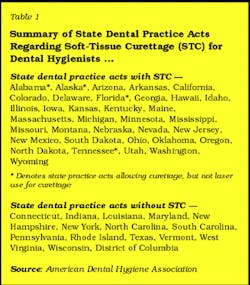
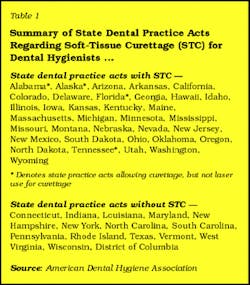
While this federal regulatory agency approves use of products in the United States, not all states permit the use of lasers by dental team members. Some states do not allow auxiliaries to perform duties with lasers, even when these duties are allowed without the laser. Table 1 lists the current status of Dental Practice Acts regarding soft-tissue curettage. More than 30 states allow registered dental hygienists to perform soft-tissue curettage, some with and without a laser. Practice acts vary from state to state. The Academy of Laser Dentistry (ALD), an international organization promoting safe and effective use of lasers by dental professionals, has a committee on Regulatory Affairs that has and is willing to appear before State Boards if notified. States can choose whether or not to accept this assistance. Tennessee recently declined this offer from ALD.
null
It is puzzling why some states rule one way and others another. For example, Illinois permits hygienists to use a soft-tissue laser, following completion of approved training. However, in April 2003, Tennessee ruled to disallow the use of lasers for subgingival curettage by hygienists. The ruling was made without input by or notification of hygienists using lasers in that state prior to the ruling. For this reason, practitioners are encouraged to check their individual state practice acts.
Other U.S. national regulatory organizations provide guidance for laser use throughout all 50 states. These include the Occupational Safety and Health Administration (OSHA), part of the U.S. Department of Labor that ensures worker safety. Laser installations are subject to OSHA review, and laser safety officer appointment, documentation, protocols, and staff training is required. The American National Standards Institute (ANSI) is a nongovernmental organization that provides guidance for the safe use of laser systems by defining control measures. This organization has a component that was recently updated by dentists to address dentistry, specifically safety issues. Clinicians must provide quality oral health care based on individual state practice acts and in accordance with other regulatory bodies. It is imperative that the dental practitioner deliver competent dental care in accordance with their education, training, and clinical experience. Dental lasers will become the standard of care for assuring reproducible outcomes for many procedures; practitioners are advised to stay current with new treatment modalities.
Oral surgery procedures that require the removal of soft tissue can be achieved by vaporization (ablation) and/or cutting (incision, excision, or dissection) with the diode laser. Some of these soft-tissue applications include but are not limited to gingivectomy, frenectomy, hemorrhagic lesion removal, gingival sculpting techniques associated with implant recovering or therapy, and subgingival curettage.3 The advantages for laser soft-tissue oral surgery include improved hemostasis, reduced intraoperative and postoperative pain/discomfort, decreased postoperative swelling, eliminated need for sutures, reduced bacterial count at the wound site, reduced operator time, and versatility. Because of its versatility, this laser may be a useful alternative for soft-tissue oral surgery compared to traditional periodontal surgery.4 The disadvantages or limitations of laser surgery compared to incisions made by scalpel include slower tissue cutting, delayed healing, and reduced surgical precision.
This article presents several clinical cases for current approved uses,5,6 and the difficulty in finding clinical research applicable for the general dentist.
null
Method of action
Lasers emit a precise beam of concentrated light energy. This light is unique in that it is comprised of a single wavelength, expressed in nanometers or one billionth of a meter, measured crest to crest in the wave. The wavelength generated is based on the active medium present in the laser device and can be a solid (Nd:YAG, diode, Er:YAG) or gas (CO2 or Argon). The diode laser is considered a solid, with a semiconductor chip embedded with crystals, making the device smaller and lighter. The active medium determines the wavelength, varying by the makeup of the crystals.
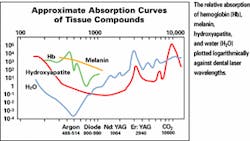
The diode wavelengths are in the near infrared spectrum, typically from 800 nm to 980 nm. The wavelength determines the absorption characteristic in biologic tissues. Absorption of laser light by biologic tissue determines efficiency of surgical removal. The various components of the biologic tissue determine whether laser light will be absorbed. Diode lasers are well-absorbed by hemoglobin and pigmented tissue and, to a lesser degree, by water. (See Table 2.) Different wavelengths are absorbed by soft tissue at varying rates, depending on the type of soft tissue.7 Keratinized tissues, containing less blood, require the use of lasers with higher wavelengths or the use of more power in general. The practitioner must match the wavelength to the specific tissue, because specific wavelengths provide great precision, minimizing potential risk of lateral tissue damage.3
Interaction of the laser with tissue is a photo-thermal event, in which light is transformed into heat. When the laser beam penetrates tissue and is absorbed, a designated amount of energy is removed per unit of time, with a resultant temperature rise. Coagulation begins at over 50°C, with protein denaturation at 60°C. At temperatures 100°C to 200°C, vaporization of water occurs. (Note: Water is the chief component of soft tissue.) Laser surgery is achieved by the process of ablation, removing this tissue by converting it to a gaseous state or plume.8 The plume is considered to be a biohazard and should be removed with high-volume evacuation.
The power output utilized by the soft-tissue diode laser is typically between .1 and 10 watts or joules per second, in a continuous output or a pulsed power.9 Diode lasers use optical fibers to deliver the laser beam. These fibers, made up of primarily quartz, can deliver light through bends and curves, therefore allowing access to difficult intraoral sites. A pencil-size handpiece glides over the fiber and locks into place. Most treatment uses direct contact with the tissue and allows the operator to experience tactile feedback similar to a scalpel or mechanical instrument.
Clinical case studies
Three clinical cases are presented. For each case, the diode laser was used at 810 nm ± 10 nm. These case studies are presented to demonstrate some soft-tissue diode treatment outcomes: Case 1 — fibroma ablation, Case 2 — soft-tissue curettage, and Case 3 — frenectomy with postorthodontic gingival recontouring. In each case, the authors received the patient's written consent and signed HIPPA consent form, and followed ANSI and OSHA guidelines. Safety precautions were observed during laser treatment — protective eyewear was worn by the operator, patient, and assistant, and the laser plume (from the ablation process) was captured via a high-volume evacuation system.
Case 1 Fibroma removal
A 58-year-old Caucasian female presented with a fibroma (2 mm x 3 mm) lower left lip at the vermilion border. Duration of the lesion was approximately four months (Figure 1). After injection of local anesthesia — 1.0 ml of 2 percent lidocaine (Septocaine, 1:100,000) — into the surrounding tissue, avoiding the fibroma, a diode laser (DioDent™, Hoya/ConBio®) at a setting of up to 2.00 watts starting at 1.00 watt in continuous mode was utilized. Postoperative instructions were provided. Packing and suturing were not used. Figure 2 — two months postoperative visit — demonstrates postoperative healing of the site with little or no evidence of prior surgery.
null
null
Case 2 Laser-assisted periodontal curettage
A 54-year-old Caucasian female presented with Type II periodontal disease (generalized 4 mm to 5 mm pockets) of unknown duration (Figure 3). All areas were charted, probed using a probe (CPITN-E probe), and treatment planned for scaling and root planing with utilization of laser in diseased areas. One manageable treatment section of scaling and root planing was conducted using 1 carpule of 2 percent lidocaine (Septocaine 1:100,000) infiltrated into the surrounding tissue. Traditional root planing and scaling were performed prior to the lasing procedure to allow improved pocket access for the fiber. A 400-micron fiber was applied directly to the diseased pocket using a light touch. Laser-assisted periodontal curettage using a diode laser (Hoya/ConBio® DioDent™ laser) at a setting of 0.6 watts in continuous wave mode in conjunction with root planing and scaling procedures were then performed.10
null
null
null
Treatment began at the gingival margin holding the fiber parallel to the tooth and slightly angled toward the diseased tissues using a deliberate, erasure-like, crosshatching motion. The fiber tip was inspected frequently to remove accumulated tissue on a 2 x 2 gauze. Typically, each pocket had a 30- to 40-second lasing treatment time, which varied depending on type of tissue and severity of disease. The procedure was evaluated as complete by evidence of a new wound site with bleeding or fresh bleed (Figure 4).8
Postoperative instructions included warm saltwater rinses twice daily and an extra-soft-bristle toothbrush to be used at next brush session. (Figure 5 demonstrates postoperative healing after one month.) Healing was assessed at a one-month recare visit where tissues appeared firm, pink, and slightly stippled. Patient was evaluated at future recare visits, and full probing was performed. Any remaining pockets over 3 mm with hemorrhage would require further lasing. In this specific case, no relasing was required.
Case 3 Gingival recontouring with frenectomy
A 15-year-old Caucasian female complained about the aesthetic result following more than two years of orthodontic therapy. Clinical examination of upper anterior teeth demonstrated hyperplastic tissue. The patient reported use of no medications (Figure 6). From Tooth #5 to Tooth #11, gingival contouring was conducted (settings were 2 watts in continuous mode) and local infiltration injections of 2 percent lidocaine, limited to soft tissue, well above bone level noted on radiograph.11 The fiber tip of the laser was applied to resect fibers of the frenum, disconnecting them from the midline.12 Figure 7 demonstrates the slight carbonization markings of the laser and hemostasis that occurred immediately after the procedure. Figure 8 demonstrates results at 20 days. The patient reported being pleased with the results.
null
null
null
Conclusion
State practice acts regulate the use of lasers in the practice of dentistry, and these vary. Practitioners should check their individual state practice acts and their own skills in utilizing lasers. This article has presented three clinical cases which illustrate the benefits of laser in soft-tissue management. These cases were selected by the authors through proper case selection, appropriate training, and a critical self-assessment of clinical skills.
The authors believe that the soft-tissue laser is a state-of-the-art tool that creates predictable aesthetic results within a general dental practice.3 The relative lack of pain, ease of use, and site specificity of the laser make it an ideal addition for therapy management.13 Comparison studies evaluating postoperative discomfort and wound closure to conventional surgery are not readily available. Multiple challenges exist for enhancing collaboration between the research community, manufacturers, and clinicians. The Academy of Laser Dentistry is bridging these gaps and may be reached at www.laserdentistry.org.
Note: The authors wish to thank Dr. Janet Hatcher Rice for her thoughtful input and advice. For additional laser information, be sure to see Drs. Jean Furuyama and Janet Hatcher Rice in Nashville, Tenn., at the AAWD annual meeting. (See Chronicle section)
References
1 Manni, J Dental Applications of Advanced Lasers, Burlington MA JGM Associates, 2000, 8-1-8-4.
2 Sulewski JG Historical Survey of Laser Dentistry. Dent Clin of North Am 2000 Oct 44(4) 7178-752.
3 Research, Science and Therapy Committee of the American Academy of Periodontology. Lasers in Periodontics. J Periodontol. 2002 Oct;73(10):1231-9.
4 Goharkhay K, Moritz A, Wilder-Smith P, et al. Effects on oral soft tissue produced by a diode laser in vitro. Lasers Surg Med. 1999;25(5):407-13.
5 Pierce MC, Jackson SD, Dickison MR, King TA, Sloan P. Laser-tissue interaction with a continuous wave 3-mcm-fiber laser: preliminary studies with soft tissue. Lasers Surg Med. 2002:26(5):491-5.
6 Radz GM. Aesthetic breakthrough. Soft tissue lasers. Dent Today 2002 Dec;21(12):38-40.
7 Freedman G. Dental lasers. Dent Today. 2002 Dec;21 (12)102-7.
8 Meserendino LJ, Pick RM. Lasers in Dentistry. Chicago, IL: Quintessence Books; 1995: chap 1.
9 Coluzzi DJ. An overview of laser wavelengths used in dentistry. Dent Clin North Am 2000 Oct;44(4):753-65.
10 Coluzzi D. Lasers and soft tissue curettage: An update. Compendium. 2002;23(11A):1104-1111.
11 Kois J. Altering gingival levels: The restorative connection. Part 1. Biological variables. J Esthetic Dent. 1994;6:3-9.
12 Bullock N Jr. The use of the CO2 laser for lingual frenectomy and excision biopsy. Compend Contin Educ Dent. 1995;16:1118-1123.
13 Bader HI. Use of lasers in periodontics. Dent Clin North Am 2000 Oct;44(4):779-91.
Lori Trost, DMD
Dr. Trost created the Center for Contemporary Dentistry in Columbia, Ill., in 1989. Her practice is known for being in the technological forefront. She is a member of the ADA and AGD and consults for 3M ESPE's "Council for Innovative Dentistry." You can reach Dr. Trost at [email protected].
Karen Kaiser, RDH
Ms. Kaiser practices with Dr. Lori Trost in Columbia, Ill. She and Dr. Trost have attained Level 1 certification in lasers from the Academy of Laser Dentistry. Ms. Kaiser is currently on the 3M/ESPE Dental Hygiene Advisory Panel. You may contact her at [email protected].
MORE INFORMATION ON LASERS FOR BUSY WOMEN DENTISTS
One of the laser courses available to women dentists is the Nd:YAG laser course from Lares Research, an Academy of Laser Dentistry (ALD) Standard Proficiency Dental Laser Course Recognized Provider.
The course is a self-paced CD-ROM-based training program, which can be completed in the office or at home, followed by an in-office clinical proficiency simulation examination. Dentists must successfully complete a written test to receive the Certificate of Completion showing they have completed a Standard Proficiency Dental Laser Continuing Education Course according to the Curriculum Guidelines and Standards for Dental Laser Education using the Nd:YAG Laser. Participants earn 7 CE credits.
The Lares laser course is the first program with a distance-learning component to be recognized by the ALD. For more information, call (800) 347-3289, Ext. 1, or visit www.laresdental.com.