A paradigm shift for caries diagnosis and treatment, part 1
By Steven C. Steinberg, DDS
In the 1940s and 1950s, caries was widespread in the U.S. Today, most people have minimal caries — in fact, 20 percent of the population has 60 percent of the caries. Treating that 20 percent requires a paradigm shift. Like Einstein, whose paradigm shift built on the success of Newton, we must build on our past success. Our surgical paradigm has served us well. However, it is time to move on to a medical paradigm.
To follow a medical model, we must understand the steps of treatment planning. Step one is to decide upon a diagnosis. Step three, the final step, is carrying out a treatment plan. Step two, determining a prognosis, often seems to be skipped in dentistry. In medicine, if a patient is given a diagnosis of cancer, the next question is, "Will I die?" In other words, what is the prognosis? To prognose the caries disease process, we need to know its natural history and current epidemiology. When does caries progress? When should we intervene with treatment? Should our treatment be surgical (fillings) or medical (antimicrobials and/or fluoride)? When we add a prognosis to our diagnosis, we are ready for an improved treatment plan.
Defining dental caries
We will define caries using the following two criteria. First, caries is a bacterial infection caused by specific bacteria. Second, caries is a reversible multifactoral process of tooth demineralization and re-mineralization. In other words, caries is an infectious disease and, until cavitation, is reversible.
Bacterial infection
The bacterial infection is due to Mutans Streptococci in the early stages and lactobacilli in the latter stages. Extensive evidence using animal models indicates that caries is a communicable, transmissible, infectious bacterial disease. It also has been shown that children between the ages of six months and 30 months may become infected by salivary exchange with their mothers.
It is important to note that not only have we identified caries to be a bacterial infection, but also that specific bacteria cause it. This concept was named the specific plaque hypothesis by Loesche and replaced the nonspecific plaque hypothesis. The idea of the nonspecific plaque hypothesis is that since everyone has plaque, no diagnosis is necessary — everyone must be treated. The goal of treatment becomes the complete removal of plaque. Since plaque forms continuously, treatment must be continuous, every day. The recall appointment is used to diagnose surgical treatment needs. In other words, we diagnose lesions, not the infection. Failure becomes the fault of the patient. Since caries is caused by plaque, caries implies improper cleaning by the patient. This leads to our traditional surgical approach to caries. To paraphrase Anderson, treating caries by restoring cavitated lesions while ignoring the bacteria would be like treating tuberculosis by surgically removing cavitated lung tissue, prosthetically repairing the area but ignoring the bacteria.
The specific plaque hypothesis provides a modern medical paradigm of treatment. It is not all plaque but rather specific plaque that contains specific odontopathogens that cause caries. Caries now is viewed as a specific infection, not as a lesion. Diagnosis becomes essential. Only those patients at risk are treated and the goal becomes removal of the organisms. There is an endpoint to treatment. Patients are recalled to diagnose reinfection. Failure to diagnose infection is the fault of the dental team since disease is caused by the infection and we must diagnose it.
A reversible multifactoral process
The last step of the caries process, the cavitation, may be seen as an event. A process is a series of progressive and interdependent steps with dynamic activity. Since caries is defined as a process, the key question becomes, is it reversible? Can caries heal? In the early stages, dental caries is reversible. How is this possible?
The development of dental caries is a dynamic process of demineralization alternating with periods of remineralization. The bacteria in the plaque on the intact tooth surface metabolize available sugar and produce acid. That acid penetrates the solid yet microscopically permeable tooth surface, driving calcium and phosphate out of the subsurface tissue, demineralizing it. The result is an initial white spot lesion.
Since the tooth surface is intact, the reverse biochemical process can occur. Saliva buffering can reverse the low pH in the plaque and, with the raised pH, calcium and phosphate are driven back into the tooth, remineralizing it. The key is the integrity of the tooth surface. If it remains intact (noncavitated), remineralization is possible. The question then becomes, what is the prognosis? Is the lesion getting better or is it getting worse?
An active lesion is progressing towards cavitation (demineralizing). An inactive lesion is not progressing or is healing (remineralizing). Determining the prognosis of the carious lesion before cavitation is a key step. Subsurface de-mineralization eventually causes the collapse of the overlying tooth surface, creating a cavitation. At this point, a surgical intervention — a filling — must be used. Until then, medical intervention is possible.
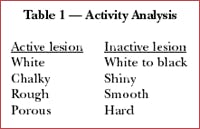
The activity status of any subsurface lesion is based on color, surface texture, and longitudinal (instead of one-time) radiographic or DIAGNOdent (KaVo America) findings. Using magnification under proper lighting and drying the tooth surface helps activity analysis. White spot lesions may be considered active sites if they appear chalky, nonglossy, and feel rough with an explorer. Inactive lesions have a relatively nonporous surface that is shiny and hard and feel smooth with an explorer. Inactive lesions may be stained to a darker color (see table 1, left).
Along with DIAGNOdent, other early diagnosis/prognosis instruments such as QLF (Quantitative Light-induced Florescence) and DIFOTI (Digital Imaging Fiber-Optic Transillumi-nation) are being introduced. It is essential that these instruments be used as part of the medical as opposed to the surgical model. Otherwise, overtreatment is possible. In assessing new instruments, the terms sensitivity and specificity must be understood. To clarify these terms think of the following example. When hiring a dental assistant, one would like that person to have both speed and quality. While the two are often mutually exclusive (more speed usually leads to less quality, more quality usually leads to a slower assistant), our goal is both. So it is with sensitivity and specificity. The sensitivity of a device is a measure of how well it finds real disease, true positive findings. The specificity of a device is a measure of how well it finds real health, true negative findings. The higher the sensitivity, the lower the specificity tends to be. The higher the specificity, the lower the sensitivity tends to be. Sensitivity is the percentage of all lesions correctly identified (false negatives detract). Sensitivity should be high with the medical/preventative paradigm (more early/benign/ reversible treatments). Sensitivity can be low with the surgical paradigm (less unnecessary, irreversible interventions). Thus a new, more sensitive device can lead to overtreatment in the surgical model. Specificity is the percentage of all sound teeth correctly identified (false positives detract). Specificity can be lower with a medical/preventative paradigm (more benign/reversible treatment so it is not bad if treating a healthy tooth). Specificity should be high with a surgical paradigm (this correctly identifies healthy teeth so less unneeded irreversible interventions occur). If surgical intervention is only needed when there is a cavitation, devices with pre-cavitation sensitivity might lead to pre-cavitation surgical intervention (fillings) where medical treatment (remineralization) is indicated.
While caries activity describes the status of the caries process as getting better or worse (demineralization/remineralization) on an individual tooth surface, caries risk describes the status of the whole patient. It can be defined as the likelihood of the patient getting a new cavitation. When educating patients, these risk factors are divided into the offense and the defense. The factors that increase the likelihood of a future carious lesion (the offense) are the bacteria levels and the sugar levels. Bacteria are necessary for caries production but are insufficient alone. Other factors are needed. Use of sugar three or more times a day between meals is considered higher risk.
The factors that lower the risk of a future carious lesion (the defense) are normal salivary flow and high levels of fluoride. Salivary flow below 0.7 ml/minute is considered a risk factor. Other risk factors are past caries history, lesion location, and medical history.
Risk categories
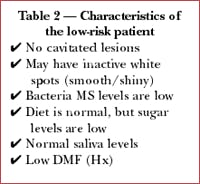
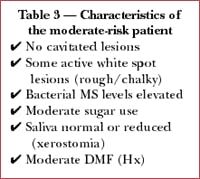
Three risk categories have been created: low, moderate, and high (see Tables 2-4). Most patients will fall into the low-risk category. These patients have no cavitated lesions, may have inactive white spots that are smooth and shiny, and no risk factors. Moderate-risk patients have no cavitated lesions but do have some active white spots or some risk factors. High-risk patients have one or more cavitated lesions. They may or may not have white spot lesions, which may be active or inactive.
Treatment
In part 2 (to be found in the September/October edition of Dental Equipment & Materials), we will discuss the medical model for caries treatment. Combining risk and activity status will give us several treatment groups. Each group will have a combined medical-surgical antimicrobial treatment protocol based on this diagnosis/prognosis.
Summary
Two key points are essential to understanding caries. First, caries is a bacterial infection caused by specific bacteria. Second, before cavitation, caries is a reversible multifactorial process of tooth demineralization and remineralization. The lesion progresses from the inside out until surface collapse (cavitation) occurs. Medical treatment of the pre-cavitated sub-surface lesion can lead to remineralization (no cavitation). Two features, caries activity and caries risk, provide a diagnosis and prognosis leading to a treatment plan protocol which will be presented in part 2 (to be found in the September/October edition of Dental Equipment & Materials).
Editor's Note: References available upon request.
Dr. Steven Steinberg has been in private practice since 1982. He has been the volunteer Director of the Ark dental clinics in Chicago. He is a clinical consultant for the University of Illinois College of Dentistry continuing-education online course on dental caries. He has spoken at the Chicago Midwinter Meeting, the Hinman Dental Meeting, and across the country on the new paradigm in the diagnosis and treatment of dental caries. He's available for speaking and can be reached at [email protected].