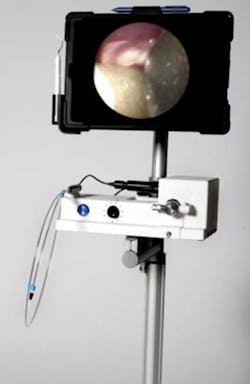
The purpose of technological advancements is to help clinicians diagnose and treat pathologies at early stages and offer enhanced procedure outcomes. Most dental practices search for technologies and procedures that will provide a competitive advantage and attract patients. One such technology is the dental endoscope (figure 1).
Dental endoscopes have been available since the 1980s. However, the image quality on early units was not very clear, which caused the first-generation units to have a steep and frustrating learning curve. We now have an endoscope with a clear, detailed image. Magnified subgingival visualization opens up a new world of advanced dentistry, with possibilities beyond using the unit as a dental hygiene tool.
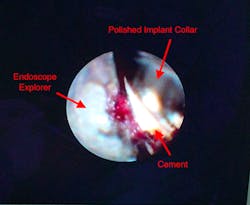
The dental endoscope captures images of the subgingival environment on a real-time, fiber optic–delivered camera. LED lighting illuminates the working area, allowing a clear image to display on either a flat-screen monitor or tablet. The image is magnified at 50x or up to 100x with new technology. The fiber locks into handles, called dental explorers (figure 2). The explorers help to retract the soft tissue and direct the light toward the working area.
Figure 1: A dental endoscope
Figure 2: A dental endoscope explorer
Once the image is displayed, the operator can remove calculus only a fraction of a millimeter in size. Ideally, the clinician holds the fiber in his or her nondominant hand and uses the camera to guide instrumentation, debriding while looking at the image. The addition of the endoscope to nonsurgical treatment may result in bone remineralization, leaving the patient in a healthy, stable periodontal state. (1) Traditional flap surgery might not be necessary if the dental endoscope is used during initial therapy.
Limiting the endoscope to use during the scaling and root planing of natural dentition is failing to take advantage of the many uses this machine has. The magnification provided by the endoscope is much greater than the magnification of the average loupe or microscope, making the endoscope a powerful diagnostic tool. Root fractures, caries, resorption, open margins, and overhanging restorations are all much easier to identify when magnified at this level. The patient can clearly see the pathosis on the screen, which makes treatment acceptance much easier to obtain.
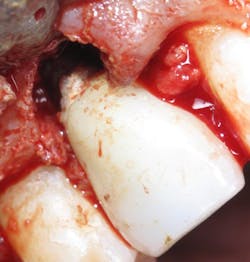
The dental endoscope is invaluable for preventing and treating peri-implantitis. The endoscope allows for visualization of residual cement, microgaps, and open and overhanging crown margins (figure 3). Inspection with the endoscope at the time of restoration can be a kind of insurance policy for the doctor to be sure that any conditions that would cause iatrogenic problems are not present (figure 4).
Figure 3: A dental implant with residual cement, as seen through the dental endoscope
Figure 4: A dental implant with residual cement during surgical repair. A dental endoscope would have shown this cement at the time of restoration, saving the patient time and money.
When treating peri-implantitis, traditional nonsurgical treatment—scaling and root planing—is an option. The recommendations for hygiene treatment around a dental implant warn hygienists to take care not to scratch or alter the implant surface. (2) This fear of iatrogenic harm, plus difficulty accessing the implant surface, may prevent hygienists from scaling adequately to remove contaminants, such as residual cement. The treatment of peri-implantitis is less traumatic to the implant when an endoscope is used. The clinician can carefully debride the implant surface, using the camera to direct his or her efforts and be certain the area has been cleared of the irritant. When an implant is debrided without the use of an endoscope, the clinician has no way to be certain that he or she is instrumenting the area with the irritant. Using an endoscope prevents overinstrumentation of the implant surface, protecting it from surface changes.
The dental endoscope can be used in a variety of ways beyond scaling and root planing, making it a versatile tool. However, the greatest benefit is the competitive advantage it brings to the dental practice. The technology appeals to patients' desire for minimally invasive yet predictable procedures. (3) Direct-to-consumer media campaigns will draw patients who are hesitant to move forward with traditional periodontal care. The addition of this technology will increase patient acceptance of recommended treatment plans, prevent iatrogenic peri-implant inflammation, and result in greater nonsurgical outcomes. The dental endoscope will position your office to be considered a technologically advanced practice by your patients and your dental peers.
Editor's note: This article is the first in a series about dental endoscopy. To read the second installment, "Visual scaling and root planing in comparison to surgical pocket reduction: A case review,"click here. This article first appeared in The Product Navigator.Click here to subscribe. Click here to learn how to submit an article.
References
1. Wilson TG Jr, Carnio J, Schenk R, Myers G. Absence of histologic signs of chronic inflammation following closed subgingival scaling and root planing using the dental endoscope: human biopsies – a pilot study. J Periodontol. 2008;79(11):2036-2041. doi: 10.1902/jop.2008.080190.
2. Gulati M, Govila V, Anand V, Anand B. Implant maintenance: a clinical update. Int Sch Res Notices. 2014;2014:908534. doi: 10.1155/2014/908534.
3. Beaudette JR, Fritz PC, Sullivan PJ, Ward WE. Oral health, nutritional choices, and dental fear and anxiety. Dent J. 2017;5(1):pii-E8. doi: 10.3390/dj5010008.
For the most current dental product articles, click here.
For the most current dental headlines, click here.
About the Author

Nicole Fortune, MBA, RDH
Nicole Fortune, MBA, RDH, is a highly-regarded dental hygienist, educator, and professional speaker who has gained industry-wide recognition for her advanced knowledge of periodontics and peri-implantitis. As a practicing hygienist, Nicole believes the best patient care happens when combining her dental hygiene knowledge with the latest technology. She holds many certifications including CO2, Diode and Nd:Yag laser certification. She is currently the only dental professional in Vermont who is certified in perioscopy. Nicole's dedication to patient care excellence, industry knowledge, and technological acumen earned her the title of Vermont’s Dental Hygienist of the Year for 2017. She is a member of many professional groups, including the Organization for Safety Asepsis and Prevention. She earned her dental hygiene degree at the University of Vermont and holds a MBA from Champlain College.
Updated June 24, 2020