Visual scaling and root planing in comparison to surgical pocket reduction: A case review
Traditionally, the most predictable treatment for moderate to advanced periodontal disease has been surgical pocket reduction, or flap surgery. Periodontal surgery with added bone regenerative materials is highly effective and predictable.
There are, however, some downsides to a surgical approach. These include potential postoperative pain and inflammation, potential temperature sensitivity, and risk of postoperative infection. Beyond the physical risks, there are other barriers for patients. These include hesitation to be referred to a specialist, cost, fear, and a desire for minimally invasive treatment. (1) For the clinician, traditional surgery requires an investment in surgical instruments, dental assistants, and regenerative materials, not to mention the opportunity cost of a patient occupying the doctor’s chair when a higher-yielding procedure could be completed using the operatory and time.
Nonsurgical treatment is effective in many early to moderate periodontal cases. However, without the surgical benefit of visualization, nonsurgical treatment is not as predictable. (2) Advanced technology now allows clinicians to use a magnified image of the root or implant structure during nonsurgical treatment. This results in a greater reduction of pocket depths and inflammation. In some cases, bone remineralization is evident after nonsurgical treatment.
The following case review is an effort to compare the efficacy of nonsurgical visual root planing completed with a dental endoscope, or Visual-SRP, to the surgical gold standard of pocket reduction surgery.
Patient presentation and clinical exam
The patient is a healthy, nonsmoking 53-year-old male with an unremarkable medical history. He takes Simvastatin and has no known drug allergies. The patient has a history of full-mouth scaling and root planing, as well as quarterly periodontal maintenance, with his restorative dentist. He has no history of periodontal surgery but had his maxillary first molars extracted due to advanced periodontal disease several years ago. His chief concern is to avoid any future extractions.
A clinical periodontal and radiographic assessment is completed. Although there is moderate bone loss in all four quadrants, his periodontal status is stable with the exceptions of Nos. 18 and 31 distal (figures 1 and 2). Both areas reveal direct distal probing depths of at least 10 mm and radiographic infrabony distal defects.
Figure 1: No. 18
Figure 2: No. 31
Many periodontists find these defects very predictable to treat with surgery and bone regenerative materials. The high peak of remaining bone provides support, blood supply, and biologic assistance to the grafted area. Conversely, this area tends to be very difficult to treat nonsurgically. Accessing the direct distal of these teeth is extremely challenging, and at depths beyond 5–6 mm, the results of the nonsurgical approach are expected to be poor.
Treatment and results
In this case, No. 18 was treated nonsurgically with Visual-SRP using a dental endoscope. The root surface was debrided using a piezoelectric scaler with left- and right-angled periodontal tips. No other adjunctive therapies were utilized for this nonsurgical treatment. On the opposite quadrant, No. 31 was treated with traditional periodontal pocket reduction surgery and bone regenerative materials. The materials used included an allograft and enamel matrix proteins.
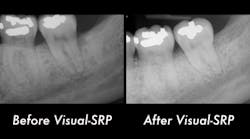
The patient returned after two weeks for a postoperative check of No. 31 and had a maintenance visit at three months post-op. At the three-month mark, the Visual-SRP area was evaluated for results. The pocket depth had resolved to 4 mm without signs of inflammation. A periapical radiograph of the area suggested bone remineralization in the site of No. 18 distal (figure 3). No. 31 was required to heal for six months and was not assessed until that time. At the six-month mark, the patient returned for another maintenance visit. The surgical area was measured, and the pocket depth had resolved to 4 mm without signs of inflammation. The periapical radiograph of No. 31 distal revealed the vertical defect was repaired, and new bone formation was evident (figure 4).
Figure 3: Periapical radiograph of No. 18 distal suggests bone remineralization, three months after nonsurgical treatment with Visual-SRP
Figure 4: Periapical radiograph of No. 31 distal shows a repaired vertical defect and new bone formation, six months after treatment with periodontal pocket reduction surgery and bone regenerative materials
This case illustrates the potential for Visual-SRP to yield results typically gained with a surgical approach. The healing time for Visual-SRP is far shorter than the healing time for surgery. This improves the oral health of the patient and, with remineralized bone, reduces the risk of recurring periodontal inflammation.
Visual-SRP is the best option for nonsurgical treatment, both for the patient and the practice. Visual-SRP is a highly technical procedure that requires clinical expertise and can be billed at a higher rate than traditional scaling and root planing. Also, the procedure is performed by a hygienist, allowing the doctor’s schedule to be filled with higher-production procedures.
Ultimately, the greatest benefit is the technologically advanced and highly skilled reputation the practice will develop with Visual-SRP. With a strong marketing campaign, patients will seek out this minimally invasive and predictable procedure.
Editor's note: This article is the second in a series about dental endoscopy. To read the first installment, "Why every office needs a dental endoscope," click here. This article first appeared in The Product Navigator.Click here to subscribe. Click here to learn how to submit an article.
References
1. Kuang Y, Hu B, Chen J, Feng G, Song J. Effects of periodontal endoscopy on the treatment of periodontitis: A systematic review and meta-analysis. J Am Dent Assoc. 2017;148(10):750-759.
2. Goodson JM, et al. Control of periodontal infections: a randomized controlled trial. J Clin Periodontol. 2012;39(6):526-536.
For the most current dental product articles, click here.
For the most current dental headlines, click here.
About the Author

Nicole Fortune, MBA, RDH
Nicole Fortune, MBA, RDH, is a highly-regarded dental hygienist, educator, and professional speaker who has gained industry-wide recognition for her advanced knowledge of periodontics and peri-implantitis. As a practicing hygienist, Nicole believes the best patient care happens when combining her dental hygiene knowledge with the latest technology. She holds many certifications including CO2, Diode and Nd:Yag laser certification. She is currently the only dental professional in Vermont who is certified in perioscopy. Nicole's dedication to patient care excellence, industry knowledge, and technological acumen earned her the title of Vermont’s Dental Hygienist of the Year for 2017. She is a member of many professional groups, including the Organization for Safety Asepsis and Prevention. She earned her dental hygiene degree at the University of Vermont and holds a MBA from Champlain College.
Updated June 24, 2020