Efficient dental implants: Incorporating 3-D printing into digital implant planning
Prosthetic-driven dental implant planning and placement form the foundation for success in implant dentistry. Dr. Murtaza Paghdiwala presents a case study that describes how a surgical guide can be planned and fabricated using CBCT technology combined with powerful planning software, and then printed from a mid-level 3-D printer in-house.
This article first appeared in the newsletter, DE's Breakthrough Clinical with Stacey Simmons, DDS. Subscribe here.
Prosthetic-driven dental implant planning and placement form the foundation for success in implant dentistry. CBCT technology combined with powerful planning software has simplified the achievement of ideal implant positioning. Incorporation of 3-D printing is the final step in taking the digital implant workflow to the mouth.
Having the proper diagnostic information can facilitate success even in less than ideal clinical presentations. CBCT scans are becoming the accepted standard of care in dental implant placement. (1) A fully limiting surgical guide based on a CBCT scan has been shown to be the superior surgical guide design. (2) Previously, the high costs associated with lab planning and lab fabrication of surgical guides forced practitioners to limit the use of guided surgery to large cases or to use inferior model-based guides. By planning and fabricating the surgical guide in-house, every implant can be placed with increased efficiency and precision.
CBCT scans are ideal for analysis of the bony architecture, but additional information is needed to accurately fabricate a 3-D printed tooth-supported guide. Scatter radiation and low resolution associated with cone beam technology create a poor image of the dentition. (3) An optical scan of the patient’s teeth, stone model, or simply a CBCT scan of a PVS impression can be used to create a digital study model. The digital model can be aligned with the CBCT scan, resulting in incredible accuracy of the bone and the dentition. The implant is placed digitally into the ideal position and a fully limiting tooth-supported guide is designed in the software and exported as a 3-D file. The guide can be printed in-house from a mid-level 3-D printer, or printed economically at a 3-D print lab.
The preoperative planning combined with a 3-D printed guide allows for easier surgery for both the patient and clinician. The guide controls drill positioning in all dimensions, including depth. This eliminates the need for sequential drilling. One implant drill can be used to create the osteotomy to the final width and depth. Research has shown no decrease in implant survivability (4) and no increase in the heat that’s generated with this method, compared to sequential drilling. (5) Surgical time decreases and patient comfort increases. A 3-D printed fully limiting surgical guide makes implant placement more efficient and more predictable.
Case study
A 37-year-old male presents with a history of trauma to the anterior mandible. At the time of the incident, teeth Nos. 26 and 27 were extracted without ridge preservation. The patient was left with large crestal and buccal defects postextraction (figures 1 and 2).
Options for ridge augmentation and delayed placement were discussed. The patient chose to have implants placed due to the existing condition of the bone, with the understanding that pink prosthetics would be necessary.
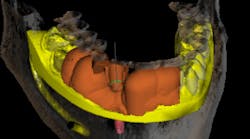
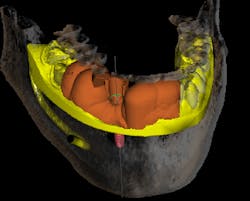
A CBCT scan was taken and imported into the implant planning software. A digital diagnostic wax-up was done by inserting teeth Nos. 26 and 27 into ideal position. With an extremely thin ridge and lack of crestal height, it was determined that space was available for a single implant. Placement was planned for a screw-retained prosthesis with an anterior cantilever (figures 3 and 4).
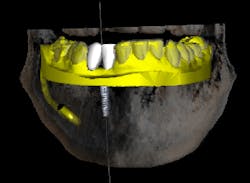
A tooth-supported fully limiting surgical guide was designed in the planning software and sent to the 3-D printer for fabrication. Once the guide was fabricated, a guide tube matching the final implant drill diameter was inserted into the guide (figure 5).
A full-thickness flap is reflected to visualize the bone and confirm positioning through the surgical guide. The guide is designed with windows to visualize proper seating. The surgical guide fully limits the implant drill in all dimensions, including depth, making it possible to drill to the final osteotomy depth and width with one drill. The implant fixture was placed and allowed to heal for four months with a healing abutment. The presurgically planned prosthesis was lab fabricated and delivered (figures 6 and 7).
The patient was pleased with the final result. A CBCT scan allowed this difficult surgical and esthetic case to be planned thoroughly beforehand. 3-D printing economically realized the planning in the actual surgery and prosthesis. 3-D printing in surgical guide fabrication allowed for more efficient and precise implant placement and restoration (figures 8 and 9).
Areas for further development in 3-D surgical guide printing include fabrication of bone-supported guides for edentulous patients and allowance for increased visualization with more translucent guide material.
References
1. Academy of Osseointegration. 2010 Guidelines of the Academy of Osseointegration for the provision of dental implants and associated patient care. Int J Oral Maxillofac Implants. 2010;25(3):620-627.
2. Kola MZ, Shah AH, Khalil HS, et al. Surgical templates for dental implant positioning; current knowledge and clinical perspectives. Niger J Surg. 2015;21(1):1-5. doi: 10.4103/1117-6806.152720.
3. Jarry G, Graham SA, Moseley DJ, Jaffray DJ, Siewerdsen JH, Verhaegen F. Characterization of scattered radiation in kV CBCT images using Monte Carlo simulations. Med Phys. 2006;33(11):4320-4329.
4. Bettach R, Taschieri S, Boukhris G, Del Fabbro M. Implant survival after preparation of the implant site using a single bur: a case series. Clin Implant Dent Relat Res. 2015;17(1):13-21. doi: 10.1111/cid.12082.
5. Bulloch S, Olsen RG, Bulloch B. Comparison of heat generation between internally guided (cannulated) single drill and traditional sequential drilling with and without a drill guide for dental implants. Int J Oral Maxillofac Implants. 2012;27(6):1456-1460.
This article first appeared in the newsletter, DE's Breakthrough Clinical with Stacey Simmons, DDS. Subscribe here.