Are you more than just thirsty? The dangerous impacts of dehydration
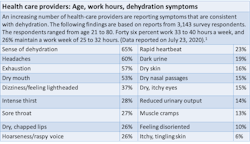
The physical environment in the dental office is more taxing than ever. A growing number of health-care professionals are experiencing profound and wide-ranging health complications since returning to the work setting. As of July 23, 2020, 65% of over 3,200 health-care providers back in active practice report dehydration. Out of 65 symptoms, dehydration tops the list as the most reported symptom.1
An increasing number of dental health-care workers are experiencing blackouts while delivering patient care, ending up in emergency rooms, and having trouble keeping awake or finding it hard to remember their daily driving route. Dehydration can contribute to each of these dangerous situations.
Water—a basic human need
The human body is an amazing machine, but like any refined piece of equipment there are physical parameters and limits that simply have to be respected. Water makes up 60% of the human body. Every organ in the body contains a large amount of water: 73% of the brain and heart tissue, 83% of the lungs, and 64% of human skin. The body human body needs water to function properly.2
Dehydration occurs when the human body loses more fluid than it takes in, creating a mineral imbalance, which affects the way the body functions.3-5 The average human male needs to consume about 3.2 quarts of water a day, while the average female requires 2.3 quarts. 2 There are a number of reasons for dehydration but excessive perspiration, and insufficient fluid intake top the list. Dehydration is commonly triggered by excessive heat. 3-5
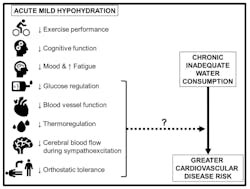
On the surface, dehydration may not seem like a big issue. In an otherwise healthy body, it is unlikely that a short period of dehydration will have a long-standing impact, but chronic or extended episodes of dehydration are simply a different matter. Dehydration impacts the brain, kidneys, circulation, respiration, and blood pressure, so getting dehydrated sets the stage for a wide range of serious physical conditions.6-12
What are we doing differently?
Many dental professionals are simply working differently now than they were at the first of the year. According to a recent survey of health care providers, workers are practicing with multiple layers of respiratory personal protective equipment (PPE). Most find the added layers of PPE very hot. Out of 3,291 survey respondents, 27% report using a respirator-level mask covered by a surgical mask, 26% wear a surgical mask and a face shield, and 56% use a three-part combination: a face shield, a respirator mask, and a surgical mask.1 In 2016, Johnson published a lengthy report detailing the extensive impact of wearing respirator masks for protracted periods of time. The study stated that more time needs to be allowed for workers performing tasks while wearing respirators and some workers cannot tolerate the breathing demands or the hot, humid conditions created when using a respirator.13
Not only are workers using more levels of protection than before the COVID 19 outbreak, 62% report only removing their PPE during their lunch break. Seven percent never remove their PPE devices during their entire work shift. To further compound the potential for dehydration, some workers are not drinking fluids throughout the day. Others are restricting their fluid intake. Some workers report it is too much of a hassle to remove PPE for a restroom break and others simply do not having enough time during the clinical day or are not allowed to take a break during their work shift. 1 These accommodations are particularly troublesome for those who are pregnant or nursing, conditions which require increased fluid intake. Lack of regular and sufficient hydration is also problematical for clinicians who have medical challenges.14,15
Additional risk factors
Dehydration is not just a summer issue. Mechanical regulation of indoor temperatures via air-conditioning and heating units play a role. Any well-designed air-conditioning unit that is operating adequately decreases humidity levels. Lower humidity is a critical factor in temperature comfort, especially in hot, humid climates. Central heating units also reduce humidity. These environmental manipulations increase the risk for dehydration.
Temperature regulation is also a critical component. There are offices where there are ongoing thermostat wars. And there are business owners who keep the settings too high to provide adequate cooling. Some air-conditioning systems simply are not robust enough to provide adequate temperature control. Working in a hot environment can be dangerous to workers. The human body is built to regulate temperature challenges, but it can be overtaxed by profuse sweating and insufficient hydration. While fans can improve air circulation, continuous air movement causes evaporation, which can also contributes to dehydration.
Outdoor environmental factors also play a role. Climates with low relative humidity levels increase the risk for dehydration. Airborne dust particles, windy climates, and air quality issues impact respiratory function. Pollen, mold, and mildew can create nasal congestion, which reduces healthy nasal breathing while increasing mouth breathing. There can also be an emotional component in the dehydration equation. Salivary flow diminishes when stress and anxiety put the body into a “fight-or-flight” mode.
Hydration strategies
It is important to know that the thirst mechanism lags behind actual level of hydration, so when one begins to feel thirsty, the body is already experiencing symptoms of mild to moderate dehydration.6 The longer the body is dehydrated, the more potential for adverse effects to both short- and long-term health. Hyperhydration can also occur if someone drinks too much fluid, but this seems improbable in today’s clinical setting.
Regular hydration is a key step.2-5,9,15 While it may be hard, it is critical to drink sufficient fluids before and after work and during any breaks. Many are turning to liquid products that claim to support or enhance hydration. Be aware that many products have very low pH levels, and often have high titratable acidity levels, factors that increase the risk for caries and erosive tooth wear.16-18
Energy drinks and sports drinks are other popular options that have hidden consequences. Many are formulated with high levels of caffeine, various sugars, and a high sodium content, which can have a negative impact on the kidneys.19 Caffeine and alcohol consumption also contribute to dehydration.3-5 Some recommend fruit-infused water or water with a slice of lemon or lime, but even a small squeeze of juice drops the overall pH to an erosive level.Iced herbal teas offer a refreshing alternative and can be sweetened by polyols like xylitol or erythritol.Nutritional intake is important. Lighter meals are recommended. Fresh fruits and vegetables, and dairy products such as yogurt all have high levels of moisture and can contribute to overall all daily fluid intake. 3-5 Frozen fruit slices or grapes are a cooling treat and offer good nutritional value. Highly processed foods and most fast food products typically contain large amounts of salt. Salt is a preservative and extends shelf life, and it is used as a flavor enhancer, but excessive intake contributes to dehydration. So instead of reaching for a traditional snack such as potato chips, look for products that are either sodium free or have no added sodium.20 The transition may be hard at first but adopting a lower sodium diet will help combat dehydration, and over time it becomes apparent how much sodium is present in foods that require little preparation.
Oral comfort strategies related to dry mouth are discussed in detail in an online article published on July 9, 2020.21 There are a wide variety of products that can help stimulate saliva, keep oral pH levels at neutral, help reduce pathogenic microbes, and provide soft tissue protection. There are also over-the-counter eye drops designed to sooth dry, irritated eyes.
Staying on track
While everyone is striving to accommodate clinical schedules and stay on time, plan for hydration and rest room breaks. This is not the time to play hero. It is the time to be smart. We are not human scaling machines or tooth mechanics. We have an ethical obligation to provide quality care and that is simply not possible if our bodies are dehydrated and stressed physiologically. The human body is built for homeostasis and adequate hydration is a key part of staying healthy.
Disclaimer: The article is designed to provide information to those experiencing dehydration issues related to the increased use of PPE in the clinical setting. This is not intended to replace a medical evaluation by a licensed physician, registered nurse, or licensed nurse practitioner.
References- The water in you: Water and the human body https://www.usgs.gov/special-topic/water-science-school/science/water-you-water-and-human-body?qt-science_center_objects=0#qt-science_center_objects. Accessed July 21, 2020.
- Hydration. Information for employers and workers. Saif.com/wellness. Accessed July 21, 2020.
- Dehydration. https://www.nhsinform.scot/illnesses-and-conditions/nutritional/dehydration#causes-of-dehydration. Accessed July 21, 2020.
- Dehydration. https://www.mayoclinic.org/diseases-conditions/dehydration/symptoms-causes/syc-20354086. Accessed July 21, 2020.
- Six signs of severe dehydration and how to treat it. https://www.gohealthuc.com/library/4-signs-severe-dehydration-and-where-go-help. Accessed July 21, 2020.
- Pross N. Effects of dehydration on brain functioning: A life-span perspective. Ann Nutr Metab. 2017;70 Suppl 1:30-36. doi:10.1159/000463060
- Liska D, Mah E, Brisbois T, Barrios PL, Baker LB, Spriet LL. Narrative review of hydration and selected health outcomes in the general population. Nutrients. 2019;11(1):70. Published 2019 Jan 1. doi:10.3390/nu11010070
- Murray R. Rehydration strategies--balancing substrate, fluid, and electrolyte provision. Int J Sports Med. 1998;19 Suppl 2:S133-S135. doi:10.1055/s-2007-971978
- Watso JC, Farquhar WB. Hydration status and cardiovascular function. Nutrients. 2019;11(8):1866. Published 2019 Aug 11. doi:10.3390/nu11081866
- Ong JJY, Bharatendu C, Goh Y, et al. Headaches associated with personal protective equipment - A cross-sectional study among frontline healthcare workers during COVID-19. Headache. 2020;60(5):864-877. doi:10.1111/head.13811
- Popkin BM, D'Anci KE, Rosenberg IH. Water, hydration, and health. Nutr Rev. 2010;68(8):439-458. doi:10.1111/j.1753-4887.2010.00304.x
- Armstrong LE. Challenges of linking chronic dehydration and fluid consumption to health outcomes. Nutr Rev. 2012;70 Suppl 2:S121-S127. doi:10.1111/j.1753-4887.2012.00539.x
- Johnson AT. Respirator masks protect health but impact performance: a review. J Biol Eng. 2016;10:4. Published 2016 Feb 9. doi:10.1186/s13036-016-0025-4
- Schols JM, De Groot CP, van der Cammen TJ, Olde Rikkert MG. Preventing and treating dehydration in the elderly during periods of illness and warm weather. J Nutr Health Aging. 2009;13(2):150-157. doi:10.1007/s12603-009-0023-z
- Gauer R, Meyers BK. Heat-related illnesses. Am Fam Physician. 2019;99(8):482-489.
- Lussi A, Schlueter N, Rakhmatullina E, Ganss C. Dental erosion--an overview with emphasis on chemical and histopathological aspects. Caries Res. 2011;45.
- Schlueter N, Luka B. Erosive tooth wear - a review on global prevalence and on its prevalence in risk groups. Br Dent J. 2018 Mar 9;224(5):364-370. doi: 10.1038/sj.bdj.2018.167. Epub 2018 Mar 2.
- Carvalho TS, Schmid TM, Baumann T, Lussi A. Erosive effect of different dietary substances on deciduous and permanent teeth. Clin Oral Investig. 2017 Jun;21(5):1519-1526. doi: 10.1007/s00784-016-1915-z. Epub 2016 Jul 23.
- García-Arroyo FE, Cristóbal M, Arellano-Buendía AS, et al. Rehydration with soft drink-like beverages exacerbates dehydration and worsens dehydration-associated renal injury. Am J Physiol Regul Integr Comp Physiol. 2016;311(1):R57-R65. doi:10.1152/ajpregu.00354.2015
- How to reduce sodium. https://www.cdc.gov/salt/reduce_sodium_tips.htm. Accessed July 21, 2020.
- Respiratory PPE, dry mouth, and COVID-19: Why you need to know your own CAMBRA score. https://www.dentistryiq.com/dental-hygiene/infection-control/article/14179240/respiratory-ppe-dry-mouth-and-covid19-why-you-need-to-know-your-own-cambra-score. Accessed July 21, 2020.
ANNE NUGENT GUIGNON, MPH, RDH, CSP, a visionary thinker, has received numerous accolades over four decades for mentoring, research, and guiding her profession. As an international speaker and prolific author, Anne focuses is on the oral microbiome, erosion, hypersensitivity, salivary dysfunction, ergonomics, and employee law issues. She may be contacted at [email protected].
About the Author

Anne Nugent Guignon, MPH, RDH, CSP
ANNE NUGENT GUIGNON, MPH, RDH, CSP, a visionary thinker, has received numerous accolades over four decades for mentoring, research, and guiding her profession. As an international speaker and prolific author, Anne focuses is on the oral microbiome, erosion, hypersensitivity, salivary dysfunction, ergonomics, and employee law issues. She may be contacted at [email protected].
Updated June 26, 2020