Aerosols
WRITTEN BY Rella Christensen, PhD
Yes, dental aerosols are a concern. These airborne particles are composed of debris and microorganisms propelled into the air from the oral cavities of the many people treated throughout the day within the office.1-6 These particles range from relatively harmless to highly infectious. They are caused by the routine dental grinding and polishing and use of compressed air to drive instruments and dry operating sites.1,6 Investigators have demonstrated that dental procedures generate large quantities of very small aerosols three microns and less in size.1 These very small particles can remain suspended at the end of treatment for many hours.2 When inhaled, their small size allows penetration to the alveoli of the lower respiratory tract,7 where infectivity is greatly increased.8 Dentistry’s invisible aerosols are inhaled inadvertently by all who enter the office - clinicians, staff, patients, people accompanying patients, service people, etc.
Despite intensive media covereage of deadly respiratory infections, such as SARS and bird flu, most dental clinicians have ignored or given only casual attention to the ever present aerosols in their workplace and their implications in respiratory infections. Continual daily contact over the years with many oral cavities and their varied contents may have blunted concern by dental clinicians. Some clinicians may believe people with serious respiratory infections are too ill to present for dental procedures. However, microorganisms are shed in high numbers during the incubation phase and immediately following cessation of clinical symptoms of many diseases. During both of these times patients generally function normally and could seek dental treatment. Some dental clinicians have stated their belief that they have enhanced immunity developed over their years of practice. Yet four separate CRA surveys, conducted at five-year intervals from 1990 to 2005, show the most common reason reported by dental clinicians for missing work is respiratory infection.9-12
Today, there is a group of simple, readily available products and tactics to minimize both the number of aerosols in the dental office and clinicians’ exposure to the aerosols. Although no one measure by itself resolves the problem, all of the precautions used together can lower risk substantially to levels well below indoor environments in general. What are these products and tactics dental clinicians can implement to improve management of aerosols in their offices?
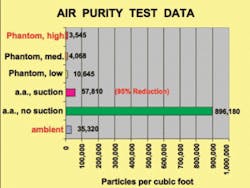
High velocity evacuation (HVE) used during all procedures - Researchers have noted the potential effectiveness of properly used high velocity evacuation (HVE) in control of aerosols. Figure 1 shows CRA data comparing aerosols present during air abrasion cutting (a.a.) with and without use of HVE and the added effect of a ceiling mounted air purifier (Phantom) used on different settings in an 8x10 foot operatory with an 8-foot ceiling. The figure shows a 95 percent reduction in aerosols due to use of HVE alone when adjusted at optimal velocity and positioned close to the operating site during a.a. use.
Almost all dental offices in the U.S. have HVE today. The critical points related to HVE in aerosol control are frequency of use and attention to aerosols. Most think of HVE to control splatter and are unaware of its value for aerosol control. Since aerosols are not generally visible, HVE is not generally used to control them. Only a change in mind-set is required to move HVE into effective use right away for aerosol control. (The foregoing information relates to use of 10mm diameter HVE tips, and a properly functioning suction pump set to evacuate one liter per minute of fluid, [Figure 2]. A saliva ejector tip has substantially less evacuation capability and is not as useful for aerosol control.)
Air purification equipment - Today, air purifiers are not used widely in dental offices, but they are potentially a very effective way to manage aerosols. Effective equipment uses high efficiency particulate air (HEPA) filters renewed at regular intervals.
CRA evaluations have shown that a ceiling mounted industrial air purifier can operate in dental operatories very efficiently (Figure 3). The efficiency of air purification is measured by the amount of time needed to process all the air in a room of a given size, and the amount and types of particles removed form the air. Due to the many small operatories with floor to ceiling walls in most dental offices, more than one unit is needed for the efficiency necessary. Unfortunately, many so-called air purifiers do little more than create noise and wind.
So, beware dental clinicians! Seek factual, objective information before you purchase. CRA has tested some equipment, the best of which is shown in Figure 3. An efficient air purifier can remove odors and pollens from the office air, as well as airborne microorganisms and debris. In the absence of air purification, good ventilation with fresh air moved through the office constantly can be useful. However, most offices today are sealed, with ability to open few to no windows. Some central heating-air conditioning systems can be designed to filter the air also, but these are costly and best installed during construction of the building.
Rubber dam use whenever possible - Rubber dam isolates the teeth to be treated from the saliva and soft tissues and tongue of the oral cavity and thereby reduces the number of microorganisms in the aerosols generated during treatment (Figure 4). This is in addition to the value of rubber dam in providing a dry field and increased access and visibility for restorative work. Rubber dam should be used routinely on every patient whenever possible.
Chlorhexidine mouth rinse before and during treatment - CRA data show two consecutive 30-second rinses with one of the commercially available 0.12 percent chlorhexidine mouthrinses (Figure 5) before dental procedures lowers the number of viable microbes before treatment.
Two consecutive rinses are needed for optimal effectiveness. The first rinse mainly complexes with the saliva and the second rinse, performed immediately after expectoration, provides the main effect in lowering microbe counts. We believe this simple procedure should become the routine as each patient is seated in the operatory before any dental procedure, and intermittently during oral hygiene procedures and any other procedures where the rubber dam cannot be used.
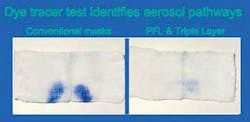
High filtration face mask with periphery that adapts to facial contours - All face masks do not protect from aerosols equally well, and face shields do not provide any protection from aerosols, but block spatter well.13 The problem with face shields is lack of fit to facial contours. Using a blue dye to test face mask and face shield efficiency, CRA found two criteria must be met:
- High filtration capability of mask material itself (at least 98-99 percent filtration of particles three microns in size)
- Close fit to the face all the way around the mask’s periphery.13
Of over 50 face masks tested by CRA so far, only two meet both the criteria. They are the PFL by AlphaProtec and the Triple Layer by 3M ESPE (Figure 6). All the other designs and brands fall short as demonstrated by the passage of the blue dye to the nostrils of human test subjects (Figure 7).13
It is important to note that all face masks must be discarded after 20 minutes of use in a high humidity environment (i.e., during cutting or polishing with a water cooled instrument) and after 60 minutes in a low humidity environment (i.e., adjusting a denture or scaling teeth) due to the invisible soak through of aerosolized liquids to the interior side of the mask.13 This soak through, referred to as wicking, draws microbe laden liquid into direct contact with the mucous membranes of the clinician’s nose and lips on the interior side of the mask. Hence, there is more involved in face mask brand choice and use than is generally considered by clinicians.
Barrier protection such as eye covering, protective clothing, and surgical cap over hair - Aerosols go everywhere in the dental operatory, but are most dense in a semicircle about 36 inches in front of the patient’s face, from ear to ear. Unfortunately, most clinicians prefer to operate within this critical zone. Placing a barrier between the clinician’s body and the settling aerosols and splatter is an easy protective strategy. Eyeglasses with side shields, a face shield plus a face mask, clinical clothing with high collar and long sleeves, and use of a surgical cap prevent aerosols from settling on hair, skin, mucous membranes, and street clothes.
Most clinicians use the barriers mentioned routinely. The only question is their design. Does the design chosen cover all the exposed parts of the clinician’s body? The clinician must decide if the barriers worn are for a show of infection control or for true protection of the exposed body parts and street clothes.
When truly effective products are chosen and employed, effective aerosol control can be achieved. Dental clinicians need to keep two important points in mind when considering dental office aerosols:
- Dental procedures inadvertently generate aerosols containing organisms and debris from each patient’s oral cavity and these can be harmful to others.
- All who enter the office must breathe the dental office air continuously in order to sustain life.
Let’s strive to minimize dental aerosols using all the methods available to us.
References
- Pollok NL III, Shay DE, Williams GH III. Evaluation of airborne contamination in a dental school clinic. J. Baltimore Coll Dent Surg 1972; 27:4-20.
- Larato DC et al. Effect of a dental air turbine drill on the bacterial counts in air. J Prosthet Dent 1966; 16:758-765.
- Belting CM, Haberfelde GC, Juhl LK. Spread of organisms from dental air rotor. JADA 1964; 68:34-37.
- Travaglini EA, Larato DC, Martin A. Dissemination of organism-bearing droplets by high-speed dental drills. J Prosthet Dent 1966; 16:132-139.
- Micik RE et al. Studies on dental aerobiology: I. Bacterial aerosols generated during dental procedures. J Dent Res 1969; 48:49-55.
- Holbrook WP et al. Bacteriological investigation of the aerosol from ultrasonic scalers. Br Dent J 1978; 144:245-247.
- Chan TL, Lippmann M. Experimental measurements and empirical modeling of the regional deposition of inhaled particles in humans. Am Ind Hyg Assoc J 1980; 41:379-409.
- Day WC, Berendt RF. Experimental tularemia in Macaca mulatta: relationship of aerosol particle size to the infectivity of airborne Pasteurella tularensis. Infect Immun 1972; 5:77-82.
- CRA Foundation, Use-survey - 1990. CRA Newsl 1990; 14:1-3.
- CRA Foundation, Product-use survey - 1995. CRA Newsl 1995; 19:1-4.
- CRA Foundation, Clinicians’ Preferences 2001. CRA Newsl 2001; 25:1-4.
- CRA Foundation, Clinicians’ Preferences 2005. CRA Newsl 1005; 29:1-4.
- Christensen RP et al. Efficacy of 42 brands of face masks and 2 face shields in preventing inhalation of airborne debris. Gen Dent 1991; 39:414-421.
Hot news: Respiratory infections
First SARS, which spread to 27 countries in six months, and now bird flu produced media headlines because of their deadly effects on humans. Virologists around the world have been anticipating with dread another worldwide flu infection similar in scope to the “Spanish Flu” of 1918, ever since the disappearance of the causative agent of that disaster that killed an estimated 20-60 million people worldwide.
For many months, world news agencies have been tracing the spread of bird flu and the inability of vaccine manufacturers to produce an effective vaccine and in quantities sufficient for everyone. Currently, no one knows exactly what mutations have to occur or in which genes to permit the bird flu virus to become easily transmissible between humans. This essential mutation will be the point at which a pandemic can begin.
A number of cases reported worldwide establish that the virus is transmissible from birds to humans, but so far suspected transmissibility between humans has been limited to only a few cases. Symptoms of bird flu include fever, sore throat, cough, and in several of the fatal cases, severe respiratory distress secondary to viral pneumonia. In an attempt to curtail the bird flu in Hong Kong, an estimated 1.5 million birds were destroyed within three days.
Since then, large numbers of birds worldwide have been confiscated, but the spread of the virus among birds continues, while the world waits in dread for authorities to announce that humans have become next on this virus’ agenda.