What dental professionals need to know about facial infections
Dental professionals can encounter facial infections during clinical examination of their patients. Here’s what you need to know about how these infections form and when to refer for treatment.
How do facial infections develop, and are there any early signs before development?
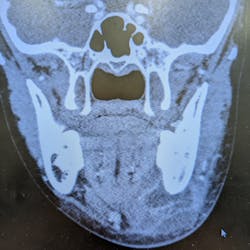
There are several reasons why, or how, facial infections develop. By far the most common is from an infected or a decayed tooth that has gone unaddressed. Over time that infection essentially seeds or extends out through the root of the tooth and then grows within the bone, until it becomes so big that it breaks through the bone and gets into the soft tissues around the face, which is when you start to notice it develop into an infection or abscess.
The second most common cause of facial abscesses are skin-related hair follicles, especially in males who shave, but it can also happen less commonly in females. This type of infection is called folliculitis.
Periodontal abscess or gingival abscess? A clinical case report
Following waterline safety fails, CDC issues rare health advisory to the dental community
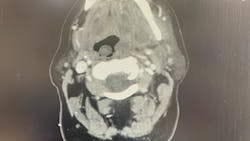
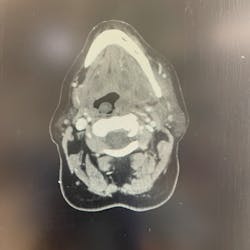
Signs of a facial infection include facial asymmetry in the form of swelling on one side of the face. The face will feel firm, warm, and tender to the touch, and redness of the skin will develop in time. It often starts with dental pain or tooth pain inside the mouth. It can also be pain inside the mouth around the tooth. As it progresses, you may see some intraoral drainage coming from the associated tooth. Infections originating from the skin will often present with external drainage. Severe odontogenic (caused by a bad tooth) infections may even spread and become so large they break through the skin.
Are there any over-the-counter medications that would help with facial infections, and at what point should patients come in for a visit?
Any type of infection or precursor to infection, which in medical terms is called cellulitis, can happen anywhere in the body, including the face and the mouth. Cellulitis includes the four cardinal signs of inflammation: calor (heat), dolor (pain), rubor (redness), and tumor (swelling).
People with signs of cellulitis require antibiotics and should seek immediate medical attention as over-the-counter medications are not strong enough or effective. Urgent care is an option as well.
Can facial infections spread anywhere else in the body, and do these sorts of infections impact vision or result in other symptoms such as headaches?
Absolutely. There’s a saying in surgery … all surgery: “never let the sun set on an abscess.” Once you have a clinical abscess, it can grow quickly and rapidly expand. It can become very dangerous in the head and neck region and is most dangerous if it spreads toward the throat. In worst-case scenarios, these infections can close the throat.
There are some spaces around the face, called potential spaces, where the fluid can collect. Some of the spaces inside the jaw and adjacent to the throat can get very dangerous. That’s why it’s important to treat facial abscesses as soon as possible, usually within 24 hours.
The most important concern with any significant facial infection is always going to be the airway. Serious and worrisome signs are when patients have difficulty breathing, difficulty swallowing or pain with swallowing, trouble breathing if they lie flat, or if they have to sit up to breathe. In these situations, the abscess is impinging on the airway.
Anyone with these types of symptoms should go to the nearest emergency room immediately. Infections around the eye can lead to periorbital edema, which, when significant, can cause the eye to become swollen shut. This usually doesn’t affect eyesight, but it can be very traumatizing and scary for patients. Very rarely an unaddressed infection can lead to blindness. Blindness from eye swelling is more common with traumatic injury and swelling than it is with infection. The good thing is that most people are going to seek treatment if their eye is swollen shut.
Conversely, a severe oral infection can also travel downward and even reach the heart. The good news is this is very rare, but those are the reasons why we must be quick to treat any kind of significant facial infection.
Is there a home remedy for facial infections?
There is no home remedy for a significant facial infection. If there is tooth pain, the sooner the patient can get to see a dentist or oral surgeon to prevent the spread of the decay or infection, the less likely they'll end up in the hospital or operating room. Make sure patients know that if they notice anything unusual on their face, it's important to see a doctor right away—e.g., a dentist, oral surgeon, primary care physician, or dermatologist.
If surgery is needed, what is the process and the procedure?
Significant facial infections that require surgery are taken care of in a hospital setting. The patient is admitted to the hospital, started on IV antibiotics and pain meds, and planned for surgical incision and drainage (commonly called I&D) often within 24 hours, based on the severity and immediate risk of spread. Patients can expect a one- to three-day hospital stay depending on their response, recovery, and need for monitoring. During the hospital stay, the patient remains on antibiotics and pain meds through an IV, both of which will be converted to oral medications upon discharge. Most surgeons also require at least one postoperative visit to check progress.
Editor’s note: This article first appeared in Through the Loupes newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles and subscribe to Through the Loupes.
About the Author

Jaclyn Tomsic, MD, DMD
Jaclyn Tomsic, MD, DMD, is an oral and maxillofacial surgeon in Cleveland, Ohio. She completed her undergraduate studies at John Carroll University in University Heights, Ohio, with a BS degree in chemistry and a minor in biology. She earned her DMD at Boston University Goldman School of Dental Medicine in Boston, Massachusetts, and she completed her oral and maxillofacial surgery training at the Detroit Medical Center in Detroit, Michigan, working at Level I trauma centers Detroit Receiving Hospital, Henry Ford Hospital, and St. John’s Medical Center. Dr. Tomsic received her medical degree from Wayne State School of Medicine in Detroit. She has extensive knowledge of jaw reconstruction, orthognathic surgery, facial plastic surgery, sleep apnea, TMJ, and dental issues. For more information, visit her website.
Updated November 9, 2022