Dental resorption: The silent killer
Editor's note: Originally published October 1, 2020. Formatting updated January 23, 2023.
So back in the day, when I was in my second year at Louisiana State University Dental School, I remember covering dental resorption in endodontics class. At the time, the common thought was that dental resorption predominantly occurs due to dental trauma. This topic took up about three paragraphs in our textbook, and then we moved on—short and sweet.
Diagnosing what it's cracked up to be: A lesson in endodontics
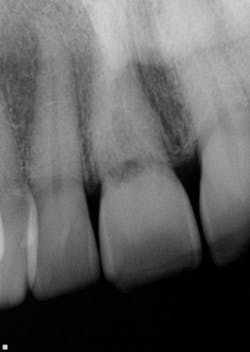
I almost missed this lesion on the radiograph
One of my referrals and I were discussing resorption one day. My colleague said he felt like he was seeing more and more cases, compared to what he had experienced over the previous 30 years. And truth be told, I have to admit the same after 22 years of practice. Obviously, this may differ from practice to practice.
Referrals have asked me many times over the years, “What do you tell patients, and how do you deal with dental resorption?”
Protocol for dealing with dental resorption
No. 1: I reassure patients that this is nothing they did or didn’t do.
It’s not caries. It’s nothing they ignored to the point of the tooth being unsalvageable. This is important, in my mind, because way too often there’s finger-pointing. But resorption is no one’s fault.
No. 2: Much like in real estate, it’s all about location, location, location.
This actually has a huge bearing on dealing with resorption. External resorption versus internal resorption—when diagnosing, it makes all the difference. In my hands (and heart), I believe the only type that stands any chance whatsoever of treatment success is internal resorption. And even then, it depends on the extent of the damage.
When evaluating and discussing external resorption, I commonly tell my patients, “I cannot make your bones and gingiva stop eating the tooth. I do not have that power.” As we have all seen, external resorption can occur in various places and teeth. However, it almost always seems to be around the area of the alveolar crest, which, in my opinion, makes restoring it almost impossible. At least with internal resorption, one has a chance. You must be aggressive in cleaning the canal way beyond the typical endo and particularly in the areas of the defect. That, my friends, is where the microscope comes in very handy.
No. 3: With resorption, it’s also about timing, timing, timing.
Unless it is caught on the early end, it does not matter. Once the resorptive damage has extended beyond a certain point, the prognosis drops precipitously, regardless of whether it started internally or externally. If communication of the defect occurs from internal to external or vice versa, I find that the prognosis goes from questionable to hopeless.
If I were to share any bit of wisdom or advice for dealing with resorption, I would leave you with this: Have a nice, long conversation with your patient about the realities and possible expectations of treating a tooth with resorption. Do not be negative. Be realistic. Let the patient make up his or her own mind. This conversation is not one to skimp on with details.
Editor’s note: This article first appeared in Through the Loupes newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles at this link and subscribe here.
About the Author
Anthony (Tony) Rainwater, DDS, MS, MEd
Anthony (Tony) Rainwater, DDS, MS, MEd, is a graduate of Louisiana State University School of Dentistry. He has master’s degrees in bacteriology and higher education. Dr. Rainwater is an endodontist who has practiced full time for the past 22 years in Lafayette, Louisiana.