Pathology case: Two patients with the same diagnosis but different treatment
Editor's note: Originally published May 5, 2015. Updated February 2023.
Case no. 1
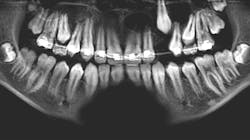
A 14-year-old female presented to her general dentist complaining of pain in the right posterior mandible and mobility of tooth no. 31. Her medical history was otherwise unremarkable. A panoramic radiograph revealed a large, multilocular radiolucent lesion within the entire ramus and posterior body of the right mandible. Tooth no. 32 was within the lesion. Cortical expansion in the area of the lesion was notable. All adjacent teeth were vital. A panoramic radiograph taken at the completion of orthodontic treatment 18 months previously showed no evidence of the lesion.
Case no. 2
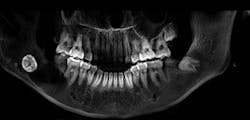
A 13-year-old male was noted by his orthodontist to have an expanding radiolucency encompassing impacted tooth no. 11. The patient was without complaint, and his medical history was otherwise unremarkable. A CT scan revealed a multilocular radiolucency extending from the maxillary midline to the area of the left permanent second molar and expanding into the left maxillary sinus. Cortical expansion in the area of the lesion was notable and all adjacent teeth were vital.
Both patients ultimately received the same histopathologic diagnosis but were treated following different protocols.
Differential diagnosis
Both of these lesions presented with a tooth within the lesion, bony expansion, and a multilocular appearance. As such, the differential diagnosis would include the keratocystic odontogenic tumor (odontogenic keratocyst), ameloblastoma, or ameloblastic fibroma. If located in the anterior region, this list would include the adenomatoid odontogenic cyst as well.
You may also be interested in...
The case of the unknown pathology
Oral symptoms of systemic pathology in a 17-year-old female
Diagnosis
Because the treatment for each of the above varies, an incisional biopsy of the lesion is necessary. In both cases, a diagnosis of keratocystic odontogenic tumor was received. Although this entity is still commonly referred to as the odontogenic keratocyst, in recent years the World Health Organization has recommended modifying the terminology to better reflect the aggressive nature of this lesion.
The keratocystic odontogenic tumor is the most aggressive and recurrent of the odontogenic cystic entities. Peak incidence is in the teens and 20s, but it may be seen at any age. The lesion may have a variety of appearances from small and unilocular to large and multilocular. The most common locations are the third molar and maxillary canine regions, but they may present throughout the jaws. This entity may also present in multiples as a component of Gorlin-Goltz syndrome.
Treatment for case no. 1
The keratocystic odontogenic tumor of the right posterior mandible was treated in the classical fashion for this entity by aggressive enucleation and curettage. Preoperatively, a 3D stereolithographic model of the mandible was obtained (figures 1-5), with the extent of the lesion defined, primarily to facilitate ease of adaptation should it be determined intraoperatively that a reconstruction plate would be required to reinforce the compromised mandible.
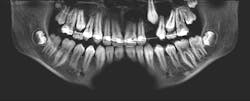
The lesion was removed via an intraoral approach and curetted from the cavity with the cyst intact. A margin of the cavity was removed using a rotary bur, and the cavity was treated with Carnoy’s solution following removal. Tooth no. 31 was noted to be intimately associated with the cyst and was removed. In four months since the surgery, repeat CBCT has demonstrated excellent bone formation within the cavity and no evidence of recurrence (figure 6).
Treatment for case no. 2
The keratocystic odontogenic tumor of the left maxilla presented a much more complicated scenario for this patient as complete removal via enucleation and curettage would require removal of permanent teeth nos. 9–15, and most of the associated alveolus. The floor of the maxillary sinus was obliterated by the cyst as well, so complete removal in this fashion would have resulted in a near hemimaxillectomy, producing a catastrophic defect for this patient. This defect would not have been just physically difficult to endure, but given the patient’s age, psychologically devastating as well.
These factors prompted a decision to treat this lesion with marsupialization, with a plan to later enucleate any residual lesion. Marsupialization involves opening the cavity of the cyst and suturing the lining to the oral mucosa, creating a permanent opening from the cyst cavity into the oral cavity. Once this is complete, the cyst will typically slowly decrease in size via appositional bone formation at the periphery of the cavity. Once the cavity has sufficiently decreased in size, the remaining lesion can be removed via enucleation and curettage as described in the first case.
At the time of publication, the lesion described had reduced in size dramatically, now extending from tooth nos. 10–12. The floor of the maxillary sinus ossified as well. The time elapsed since the marsupialization procedure was six months. Removal of the residual cyst with immediate bone grafting would be performed shortly, likely including the sacrifice of the lateral incisor and second bicuspid. Although this is a large defect, it will be much more easily managed than that posed if marsupialization had not been utilized (figure 7).
Conclusions
In the management of pathologic lesions of the head and neck region, appropriate management is often dictated by the diagnosis. Occasionally, however, options exist that can decrease the negative impact on the patient both physically and psychologically.
About the Author

R.F. John Holtzen, DMD
R.F. John Holtzen, DMD, is a board-certified oral and maxillofacial surgeon with private practices in Missoula, Montana, and Las Vegas, Nevada. He is a graduate of Temple University School of Dentistry, and completed internship and residency programs at Johns Hopkins University, St. John’s Mercy Medical Center, and MCP-Hahnemann University Medical Centers. He is a previous associate clinical professor at the University of Nevada School of Medicine and has lectured on a variety of topics related to his specialty. Dr. Holtzen is a diplomate of the American Board of Oral and Maxillofacial Surgeons, a diplomate of the American Board of Dental Anesthesiology, and a fellow of the International Association of Oral and Maxillofacial Surgeons.