Dr. Stacey Gividen, editorial director of Breakthrough Clinical, shares her story about how she was duped by a patient with a drug habit. She has insider's advice from pharmacists and others about drug seekers and their strategies, how to protect yourself from them, and the very latest guidelines for prescribing opioids and narcotics.
Editor's note: This article first appeared in DE's Breakthrough Clinical, the clinical specialties newsletter created just for dentists. Browse our newsletter archives to find out more and subscribe here.
50 OXYCODONE. TWO DAYS. THREE DIFFERENT PROVIDERS. Those were the statistics for the patient who presented to my office with a chief complaint of severe pain and tenderness on the left side of his jaw—so much so that palpation and any attempted acquisition of radiographs were met with groaning, wincing, and an increased rate of breathing. In short, the area was “hot.”
In the course of obtaining clues to the puzzle, the patient’s answers were perfectly scripted and I wanted to give him the benefit of the doubt. Who wouldn’t? Due to the unclear diagnosis (it appeared to be soft tissue ... possibly an infected parotid gland? ... definitely not black and white), I referred the patient to an oral surgeon. And yes, I prescribed pain meds (oxycodone) to get him by—20 of them.
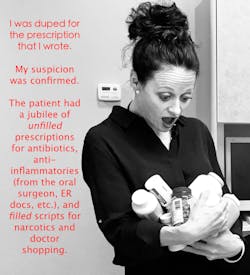
I was duped for the prescription that I wrote, but I didn’t really consider that a possibility until the next day when the patient called wanting even more meds, because the ones I gave him “upset his stomach.” Stomach sensitivity isn’t unusual with narcotics, so, once again, I gave him the benefit of the doubt and called in a small script of tramadol. He became upset when he didn’t get his requested narcotics, and that was when I started to see a few small red flags. But I didn't think about it too much because it was Thursday afternoon and I was wrapping up my schedule; this patient would be seen by the oral surgeon the next day anyway. I definitely wasn’t going to give him more opioids. I considered the situation out of my hands, for the most part, and what more could I do?
I didn't give it another thought until the following Monday, when I asked my front desk staff to follow up to see if the patient had been seen by the oral surgeon. Interestingly, every single one of the patient's numbers had been disconnected, even his emergency contact. Really? OK, BIG red flag. Subsequently, my curiosity got the better of me, so I picked up the phone and called my local pharmacist buddies to get their side of the story.
My suspicion was confirmed. The patient had a jubilee of unfilled prescriptions for antibiotics, anti-inflammatories (from the oral surgeon, ER docs, etc.), and filled scripts for narcotics he'd obtained while doctor shopping. Insert angry emoticon here.
If you’ve never had something like this happen, then I give you big kudos and a huge fist bump—I am not one of those people nor has the aforementioned scenario been my first experience. I admit this because after 14 years of practice, it’s inevitable that drug seekers will find their way to my office. I’ve caught several in their attempts (yay!), but every now and then, they say the right things at just the right time, and I become a victim of their habit simply because I have a DEA number.
Let’s view it from a different perspective—that of the pharmacists'. Here are some tidbits I have learned.
⚫️If you live near the border of another state, know that patients easily cross state lines to fill their scripts, because it doesn’t show up on their home state's drug registry. There are, however, savvy pharmacists who are licensed in both states who can access this information for you! Find out who they are and give them a jingle if you have questions or are suspicious.
⚫ In general, pharmacists don’t like to question a physician’s prescribing regimens, but the information they can access (i.e., prescription histories that are linked via drug registries) easily allows us to “catch a patient in the act.” So, if you do get a call from your pharmacist, listen to what he or she has to say.
⚫ Many pharmacies (such as Walgreens) will require the pharmacist to look up a patient's name on the registry if he or she is getting a narcotic or specific medication filled (e.g., oxycodone, methadone, etc.). This requirement often tips off the pharmacist (and us) as to who the drug seeker is.
⚫ Pharmacies update their registry systems at different times per script (daily, weekly ...) and some via computer, some manually. So, if a patient is drug seeking and fills a script, the prescription history may not show up until later, which allows the patient to have multiple fills in a short period of time without being caught. Hmm ... I never thought of that!
⚫ A trick a drug seeker sometimes will employ is to use a different name—for example, Nick versus Nicholas. All of the other information can be the same (birthdate, last name, etc.), but the computer system will see the record as two different individuals. Gotta be diligent with this one!
Now, let's look at a few numbers. How about these staggering statistics?
⚫ Studies have revealed that more than 75 million Americans (that's 25% of the entire population) have chronic or recurrent pain. (1)
⚫ Drug overdose deaths have nearly quadrupled from 1999–2014. (2)
⚫ Between the years of 1999 and 2010, the quantity of prescription opioids sold to doctors' offices, pharmacies, and hospitals has almost quadrupled, but the amount of pain that Americans have reported has stayed nearly the same. See first bullet point. (3)
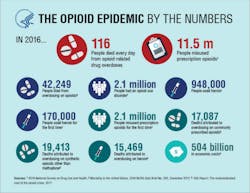
⚫ And here are some eye-opening numbers taken from the US Department of Health and Human Services: (4)
Yeah, Houston, we’ve got a problem.
Is there anything I would have done differently regarding this patient? No doubt many of you read my account and went through your own critique. That’s why I put it all out on the table, folks. We’re not perfect! We all know hindsight is 20/20. In retrospect, I would have called the pharmacy and inquired about the patient's prescription history before calling in pain meds. His anger at being denied another narcotic script was a definite giveaway, and I let my busy schedule get the better of me. Furthermore, I generally never write scripts for more than 10 to 12 pills at a time. So why did I give 20 pills to this patient? I’m still ruminating over that one and kicking myself for it too. However, since I’m a glass-half-full kind of person, I am taking this as a learning point for myself and a teaching point for you, my readers.
I’ll submit that the issue at hand requires all of us health-care providers to collaborate and communicate with each other regarding suspicious patient behavior. Pharmacists are key in this equation, as is our clinical ability to recognize those red flags that will get waved, even if in an oh-so-subtle way.
Want some good, quick advice? This online brochure: "Don’t be scammed by a drug user" from the US Department of Justice Drug Enforcement Agency's (DEA) Diversion Control Division has helpful tips on how to spot drug seekers. I love, love, love this review. Check it out; it takes less than five minutes to read.
And here is another great resource that you will definitely appreciate: Guideline for Prescribing Opioids for Chronic Pain. It's hot off the press from the Centers for Disease Control and Prevention/DEA.
This problem ... this epidemic ... is not going away, and we are right in the line of fire. I’d love to hear your stories, your experiences, and any protocols you follow with regard to this issue. Let's help each other. Let's connect. We are, after all, here for each other.
Cheers!
Stacey L. Gividen, DDS
Editorial Director, DE’s Breakthrough Clinical
LAST MONTH ...
>> You're from Montana, and you're not as good as my dentist in California'
MORE ABOUT OPIOIDS ...
>> Opioid addiction: 4 ways dentists can help solve the national epidemic
References
1. Manubay JM, Muchow C, Sullivan MA. Prescription drug abuse: Epidemiology, regulatory issues, chronic pain management with narcotic analgesics. Primary Care: Clinics in Office Practice. 2011;38(1):71-90.
2. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(50-51):1445-1452. doi: 10.15585/mmwr.mm655051e1. Erratum: 65(50-51). MMWR Morb Mortal Wkly Rep. 2017;66:35. doi: 10.15585/mmwr.mm6601a10.
3. Drug overdose deaths in the United States continue to increase in 2016. Centers for Disease Control and Prevention website. National Center for Injury Prevention and Control. Division of Unintentional Injury Prevention. https://www.cdc.gov/drugoverdose/epidemic/index.html. Updated August 30, 2017. Accessed February 18, 2018.
4. About the US opioid epidemic. US Department of Health and Human Services website. https://www.hhs.gov/opioids/about-the-epidemic/. Updated February 12, 2018. Accessed February 18, 2018.
Editor's note: This article first appeared in DE's Breakthrough Clinical, the clinical specialties newsletter created just for dentists. Browse our newsletter archives to find out more and subscribe here.
For more articles about clinical dentistry, click here.
Stacey L. Gividen, DDS, is in private practice in Hamilton, Montana. She is a graduate of Marquette University School of Dentistry. Dr. Gividen is a guest lecturer at the University of Montana in the Anatomy and Physiology Department. She is the editorial director of PennWell’s clinical dental specialties newsletter, DE’s Breakthrough Clinical with Stacey Simmons, DDS, and a contributing author for DentistryIQ, Perio-Implant Advisory, and Dental Economics. Dr. Gividen can be reached at [email protected].For the most current dental headlines, click here.
About the Author
Stacey L. Gividen, DDS
Stacey L. Gividen, DDS, a graduate of Marquette University School of Dentistry, is in private practice in Montana. She is a guest lecturer at the University of Montana in the Anatomy and Physiology Department. Dr. Gividen has contributed to DentistryIQ, Perio-Implant Advisory, and Dental Economics. You may contact her at [email protected].